 在 COVID-19 相关呼吸衰竭患者中验证呼吸频率-氧合指数
在 COVID-19 相关呼吸衰竭患者中验证呼吸频率-氧合指数
# 在 COVID-19 相关呼吸衰竭患者中验证呼吸频率 - 氧合指数
Validation of Respiratory Rate-Oxygenation Index in Patients With COVID-19–Related Respiratory Failure
Atman 翻译 + 未校对# 摘要
目的:呼吸频率 - 氧合 (ROX) 指数是氧饱和度、Fio2 和呼吸频率的分数,已被验证可预测接受经鼻高流量湿化氧疗 (HFNC) 患者接受有创机械通气的情况。本研究旨在验证 ROX 在 COVID-19 相关呼吸衰竭住院患者队列中的应用。
OBJECTIVES: The respiratory rate-oxygenation (ROX) index is a fraction of oxygen saturation, Fio2, and respiratory rate that has been validated to predict receipt of invasive mechanical ventilation in patients receiving high-flow nasal cannula (HFNC). This study aimed to validate ROX in a cohort of inpatients with COVID-19–related respiratory failure.
设计:ROX 指数的回顾性验证。我们计算了住院期间任何时间有创机械通气 ROX 的敏感性、特异性、阳性预测值、阴性预测值和 95% CI。
DESIGN: Retrospective validation of the ROX index. We calculated sensitivity, specificity, positive predictive value, negative predictive value, and 95% CIs of ROX for invasive mechanical ventilation any time during hospitalization.
地点:北加利福尼亚 Kaiser Permanente 的 21 家医院,一个综合医疗服务系统。
SETTING: Twenty-one hospitals of Kaiser Permanente Northern California, an integrated healthcare delivery system.
患者:我们确定了 2020 年 02 月 01 日至 2020 年 12 月 31 日住院 3 周内或住院期间严重急性呼吸综合征冠状病毒 2 聚合酶链反应检测阳性的成人。
PATIENTS: We identified adults with positive severe acute respiratory syndrome coronavirus 2 polymerase chain reaction test within 3 weeks of, or during, hospitalization between February 1, 2020, and December 31, 2020.
我们计算了 HFNC 开始后 12 小时的 ROX。
We calculated ROX at 12 hours after HFNC initiation.
我们使用以前发表的阈值将患者分为低 (≥4.88)、中(< 4.88 和≥3.85)或高 (< 3.85) 风险。
We grouped patients as low (≥ 4.88), intermediate (< 4.88 and ≥ 3.85), or high (< 3.85) risk using previously published thresholds.
干预:无。
INTERVENTIONS: None.
测量和主要结果:我们确定了 1847 例生命支持不受限的患者。
MEASUREMENTS AND MAIN RESULTS: We identified 1,847 patients who had no limitation of life support.
其中住院期间任何时间接受有创机械通气 525 例 (31.7%),死亡 511 例 (27.7%)。
Of these, 525 (31.7%) received invasive mechanical ventilation any time during hospitalization and 511 died (27.7%).
::: ::::
12 小时 ROX 阈值 (<3.85) 预测有创机械通气的敏感性、特异性、阳性预测值和阴性预测值分别为 32.3%(95% CI 为 28.5-36.3%)、89.8%(95% CI 为 88.0-91.4%)、59.4%(95% CI 为 53.8-64.9%)和 74.1%(95% CI 为 71.8-76.3%)。
The sensitivity, specificity, positive predictive value, and negative predictive value of 12-hour ROX threshold (< 3.85) predicting invasive mechanical ventilation were 32.3% (95% CI, 28.5–36.3%), 89.8% (95% CI, 88.0–91.4%), 59.4% (95% CI, 53.8–64.9%), and 74.1% (95% CI, 71.8–76.3%), respectively.
结论:对于需要有创机械通气的 COVID-19 患者,当阈值小于 3.85 时,12 小时 ROX 指数具有阳性预测值 (59.4%)。我们的卫生系统已经将 ROX 嵌入到电子健康记录中,以在住院激增期间进行优先取舍。
CONCLUSIONS: The 12-hour ROX index has a positive predictive value (59.4%) using threshold of less than 3.85 for COVID-19 patients needing invasive mechanical ventilation. Our health system has embedded ROX into the electronic health record to prioritize rounding during periods of inpatient surge.
关键词:COVID-19;机械通气;呼吸频率 - 氧合指数既往研究显示,急性低氧性呼吸衰竭患者可从通过经鼻高流量湿化氧疗 (HFNC) 输送的氧气中获益 (1)。
KEY WORDS: COVID-19; mechanical ventilation; respiratory rate-oxygenation index Prior studies show that patients with acute hypoxemic respiratory failure can benefit from oxygen delivered via high-flow nasal cannula (HFNC) (1).
# 序言
因此,HFNC 常用于治疗重度 COVID-19 肺炎患者 (2)。
Accordingly, HFNC has been commonly used to treat patients with severe COVID-19 pneumonia (2).
需要工具来预测哪些需要 HFNC 的 COVID19 患者将需要有创机械通气,以防止护理延迟并适当分配资源。
Tools to predict which patients with COVID19 requiring HFNC will require invasive mechanical ventilation are needed to prevent delays in care and allocate resources appropriately.
呼吸频率氧合 (ROX)(3,4) 指数是氧饱和度除以 Fio2 作为分子,呼吸频率作为分母的分数。
The respiratory rateoxygenation (ROX) (3, 4) index is a fraction of oxygen saturation divided by Fio2 as the numerator and respiratory rate as the denominator.
ROX 指数已被验证可预测 Laura C. Myers,MD,MPH1,2 Dustin Mark,MD2 Brett Ley,MD2 Michael Guarnieri,MD2 Melinda Hofmeister,BS ha,RRT3 Shirley Paulson,DNP,MPA,RN,NEA-BC4 Gregory Marelich,MD2 Vincent X. Liu,MD,MS1,
ROX index has been validated to predict receipt of invasive mechanical ventilation in patients Laura C. Myers, MD, MPH1,2 Dustin Mark, MD2 Brett Ley, MD2 Michael Guarnieri, MD2 Melinda Hofmeister, BS HA, RRT3 Shirley Paulson, DNP, MPA, RN, NEA-BC4 Gregory Marelich, MD2 Vincent X. Liu, MD, MS1,
2 在存在 COVID-19 前因任何原因接受 HFNC 的 COVID-19 相关呼吸衰竭患者中验证呼吸频率 - 氧合指数 (3)。
2 Validation of Respiratory Rate-Oxygenation Index in Patients With COVID-19–Related Respiratory Failure receiving HFNC for any cause before COVID-19 existed (3).
之前的一项前瞻性验证研究显示,随着从开始 HFNC 的时间增加(2、6 和 12 h),ROX 指数具有更好的性能,可用于识别低危和高危患者 (3)。
A previous prospective validation study showed that ROX index had better performance with increasing time from initiation of HFNC (2-, 6-, and 12-hr) and could be used to identify both low- and high-risk patients (3).
评价 ROX 在 COVID-19 中性能的数据有限。
Data evaluating performance of ROX in COVID-19 is limited.
我们的目的是在接受 HFNC 的大型 COVID-19 患者队列中验证 ROX。
We aimed to validate ROX in a large cohort of COVID-19 patients receiving HFNC.
# 方法
方法:我们确定了在综合医疗保健系统 Kaiser Permanente Northern California 的 21 家医院中,2020 年 02 月 01 日至 2020 年 12 月 31 日住院前 3 周内或住院期间严重急性呼吸综合征冠状病毒 2 聚合酶链反应检测阳性的成人(≥18 岁)。
METHODS
We identified adults (≥ 18 yr) with a positive severe acute respiratory syndrome coronavirus 2 polymerase chain reaction test within 3 weeks prior to, or during, a hospitalization between February 1, 2020, and December 31, 2020, across 21 hospitals of Kaiser Permanente Northern California, an integrated healthcare delivery system.
我们将范围缩小至接受 HFNC 氧气的患者。
We narrowed to patients receiving HFNC oxygen.
如果患者需要有创机械通气,则在插管前必须有大于或等于 1 次 HFNC 记录。
If patients required invasive mechanical ventilation, they had to have greater than or equal to 1 HFNC recording before intubation.
我们根据 HFNC 启动前的代码状态顺序排除了生命支持受限的患者。
We excluded patients with limitation of life support based on code status order before HFNC initiation.
我们决定不排除在 HFNC 开始前后接受无创通气的患者,因为目标是确定 ROX 的准确性,无论是否输送无创通气。
We decided not to exclude patients who received noninvasive ventilation before or after HFNC initiation because the goal was to determine accuracy of ROX regardless of whether noninvasive ventilation was delivered.
对于每例患者,我们计算了 ROX 指数,选择最接近但早于 HFNC 开始后 12 小时时间戳的值 (3)。我们选择了 12 小时时间点,因为 1)ROX 随时间推移更准确 (3),2)12 小时后死亡增加 (3)。
For each patient, we calculated ROX index, choosing the value closest to, but preceding, the 12-hour timestamp after HFNC initiation (3). We chose the 12-hour timepoint because 1) ROX is more accurate over time (3) and 2) death was shown to increase after 12 hours (3).
我们根据既往研究将患者分为低 (≥4.88)、中(< 4.88 和≥3.85)或高 (< 3.85) 风险 [3]。
We grouped patients as low (≥ 4.88), intermediate (< 4.88 and ≥ 3.85), or high (< 3.85) risk according to previous studies (3).
我们使用两个风险阈值(< 4.88 和 < 3.85)计算了住院期间任何时间有创机械通气 ROX 的敏感性、特异性、阳性预测值、阴性预测值和 95% CI。
We calculated sensitivity, specificity, positive predictive value, negative predictive value, and 95% CIs of ROX for invasive mechanical ventilation any time during hospitalization using two risk thresholds (< 4.88 and < 3.85).
我们按风险组评价了 1)HFNC 开始后 24 小时内有创机械通气,2)住院期间任何时间有创机械通气,或 3)住院死亡的患者百分比。
We evaluated the percent of patients by risk group who had 1) invasive mechanical ventilation within 24 hours of HFNC initiation, 2) invasive mechanical ventilation anytime during hospitalization, or 3) inpatient death.
为了证实 ROX 风险组与后续临床结局风险之间的关系,我们建立了 Cox 模型。
To confirm the relationship between ROX risk group and risk of subsequent clinical outcome, we developed a Cox model.
暴露为 ROX 风险组,结局为有创机械通气或死亡。
Exposure was ROX risk group and outcome was invasive mechanical ventilation or death.
如果患者存活出院,我们对其进行删失。
We censored patients if discharged alive.
我们报告了未校正 / 校正的风险比 (95% CI),以低风险组作为参考。
We report unadjusted/adjusted hazard ratios (95% CI) with low-risk group as reference.
协变量包括年龄、性别、合并症点评分第 2 版 (5)、生命体征(心率、血压)、疾病严重程度评分(Epic 恶化指数)和实验室检查值(血气、碳酸氢盐、肌钙蛋白、d - 二聚体)。
Covariates included age, sex, Comorbidity Point Score, version 2 (5), vitals (heart rate, blood pressure), severity of illness score (Epic Deterioration Index), and laboratory values (blood gas, bicarbonate, troponin, d-dimer).
Epic 恶化指数(范围:0-100)是 Epic 开发的经验证的疾病严重程度评分,基于临床数据,包括生命体征、实验室检查值和护理评估。
Epic Deterioration Index (range, 0–100) is a validated severity of illness score developed by Epic that is based on clinical data including vital signs, laboratory values, and nursing assessments.
北加州凯萨医疗机构机构审查委员会批准了该项目 (1262727-51),免除了知情同意的需要。
The Kaiser Permanente Northern California Institutional Review Board approved the project (1262727-51), waiving the need for informed consent.
我们使用 STATA/SE 14.2 (StataCorp LLC,College Station,TX)。
We used STATA/SE 14.2 (StataCorp LLC, College Station, TX).
# 结果
结果:我们确定了 2,039 例接受 HFNC 的患者,包括 1,847 例无生命支持限制的患者。
RESULTS
We identified 2,039 patients who received HFNC, including 1,847 who had no limitation of life support.
其中 657 例 (35.6%) 后续接受无创通气,525 例 (31.7%) 住院期间任何时间接受有创机械通气,511 例死亡 (27.7%)。
Of these, 657 (35.6%) received subsequent noninvasive ventilation, 525 (31.7%) received invasive mechanical ventilation any time during hospitalization, and 511 died (27.7%).
从入院至 HFNC 开始的中位时间为 20.8 h(四分位差 [IQR],4.1–56.1 h)。
The median time from admission to HFNC initiation was 20.8 hours (interquartile range [IQR], 4.1–56.1 hr).
基于 12 小时 ROX 值,1176 例患者 (63.7%) 为低风险,353 例 (19.1%) 为中等风险,318 例 (17.2%) 为高风险(表 1)。
Based on the 12-hour ROX value, 1,176 patients (63.7%) were low risk, 353 (19.1%) were intermediate, and 318 (17.2%) were high (Table 1).
在接受有创机械通气的患者中,从开始 HFNC 至有创机械通气的中位时间为 83.5 h (IQR,27.8-178.9 h)。
Among those receiving invasive mechanical ventilation, median time from HFNC initiation to invasive mechanical ventilation was 83.5 hours (IQR, 27.8–178.9 hr).
12 小时 ROX 阈值小于 4.88 预测有创机械通气的敏感性、特异性、阳性预测值和阴性预测值分别为 58.1%(95% CI 为 54.0-62.2%)、73.8%(95% CI 为 71.3-76.2%)、50.7%(95% CI 为 46.8-54.5%)和 79.2%(95% CI 为 76.7-81.5%)。
The sensitivity, specificity, positive predictive value, and negative predictive value of 12-hour ROX threshold of less than 4.88 predicting invasive mechanical ventilation were 58.1% (95% CI, 54.0–62.2%), 73.8% (95% CI, 71.3–76.2%), 50.7% (95% CI, 46.8–54.5%), and 79.2% (95% CI, 76.7–81.5%), respectively.
使用 12 小时 ROX 阈值小于 3.85 的相应值分别为 32.3%(95% CI,28.5-36.3%)、89.8%(95% CI,88.0-91.4%)、59.4%(95% CI,53.8-64.9%)、74.1%(95% CI,71.8-76.3%)。
The corresponding values using 12-hour ROX threshold of less than 3.85 were 32.3% (95% CI, 28.5–36.3%), 89.8% (95% CI, 88.0–91.4%), 59.4% (95% CI, 53.8–64.9%), 74.1% (95% CI, 71.8–76.3%), respectively.
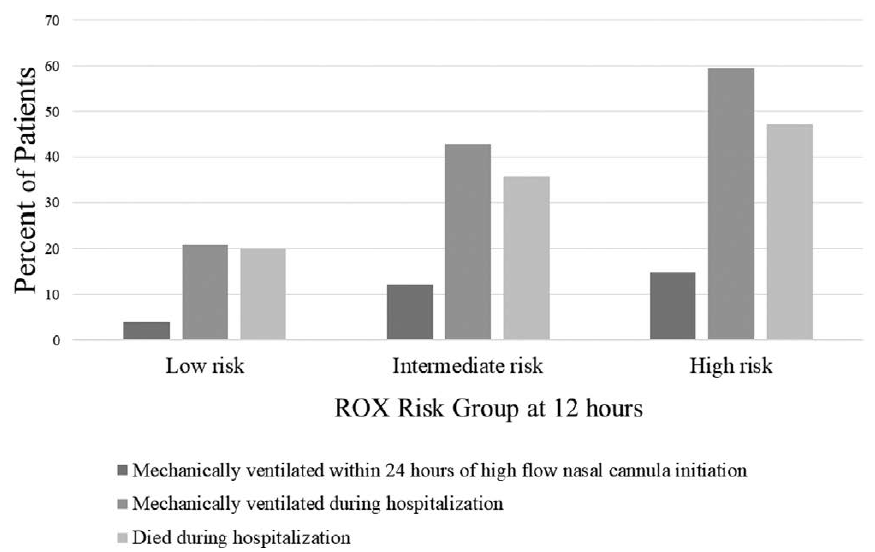
图 1 按风险组显示了 1)HFNC 开始后 24 小时内有创机械通气,2)住院期间任何时间有创机械通气和 3)死亡的患者百分比。
Figure 1 displays percent of patients by risk group who had 1) invasive mechanical ventilation within 24 hours of HFNC initiation, 2) invasive mechanical ventilation anytime during hospitalization, and 3) death.
ROX 风险组的不良结局增加。在 1,176 例低风险患者中,245 例 (20.8%)
Adverse outcomes increased with ROX risk group. Of the 1,176 low-risk patients, 245 (20.8%)
住院期间插管;353 例中危患者中,151 例 (42.8%) 在住院期间插管;318 例高危患者中,189 例 (59.4%) 在住院期间插管。
were intubated during the hospitalization; of the 353 intermediaterisk patients, 151 (42.8%) were intubated during the hospitalization; and of the 318 high-risk patients, 189 (59.4%) were intubated during the hospitalization.
同样,低危 235 例 (20.0%)、中危 126 例 (35.7%)、高危 150 例 (47.2%) 发生死亡。
Similarly, death occurred in 235 (20.0%) of low, 126 (35.7%) of intermediate, and 150 (47.2%) of high risk.
在生存分析中,与低风险相比,中风险的未校正风险比为 2.1 (95% CI,1.7-2.6),高风险的未校正风险比为 2.9 (95% CI,2.3-3.5)。与低风险相比,中风险的校正风险比为 2.2 (95% CI,1.7-2.7),高风险的校正风险比为 3.0 (95% CI,2.4-3.7)。
In survival analysis, the unadjusted hazard ratio was 2.1 (95% CI, 1.7–2.6) for intermediate risk and 2.9 (95% CI, 2.3–3.5) for high risk, both compared with low risk. The adjusted hazard ratio was 2.2 (95% CI, 1.7–2.7) for intermediate risk and 3.0 (95% CI, 2.4– 3.7) for high risk, both compared with low risk.
# 讨论
讨论:我们发现 12 小时 ROX 指数对需要有创机械通气的 COVID-19 患者有阳性预测价值(阈值 < 3.85 时为 59.4%),并且可以对患者进行早期有创机械通气和死亡的风险分层。
DISCUSSION
We found that 12-hour ROX index has a positive predictive value (59.4% for < 3.85 threshold) for COVID-19 patients needing invasive mechanical ventilation and could risk stratify patients for both early invasive mechanical ventilation and death.
该阳性预测值低于原始 ROX 验证队列 (81%)(3),这可能是由于病毒性肺炎是该队列中的罕见诊断 (~12%)。
This positive predictive value is lower than the original ROX validation cohort (81%) (3), which could be due to viral pneumonia being an infrequent diagnosis in that cohort (~12%).
在 COVID-19 激增期间,当医院面临巨大的压力时,像 ROX 指数这样的工具可以指导资源和工作人员的分配。我们的卫生系统已经将 ROX 嵌入到电子健康记录中,以识别高危患者。
During periods of COVID-19 surge, when hospitals are under tremendous strain, tools like ROX index can guide resource and staff allocation. Our health system has embedded ROX into the electronic health record to identify high-risk patients.
没有可接受的临界值来认为阳性预测值是足够的。必须在临床情境和干预成本 / 获益的背景下解释阳性预测值。
There is no acceptable cutoff to call a positive predictive value adequate. One must interpret the positive predictive value in the context of the clinical scenario and cost/benefit of the intervention.
例如,我们在《新英格兰医学杂志》的前期工作中表明,一个实施的阳性预测值仅为 10% 的模型可以与死亡率的下降相关 [6]。本研究中 59.4% 的阳性预测值与评价 (7) 1.7 所需的数量相关
For example, we have shown in previous work in the New England Journal of Medicine that a model implemented with a positive predictive value of only 10% can be associated with a decrease in mortality (6). The positive predictive value of 59.4% in this study correlates to a number needed to evaluate (7) of 1.7
(以 1 / 阳性预测值计算),作为电子筛查工具使用效果极佳,尤其是与床旁临床评估相结合时。此外,四舍五入优先次序的干预不需要任何成本,因为无论如何都会对患者进行四舍五入。
(calculated as 1/ positive predictive value), which is excellent to use as an electronic screening tool, especially when it is combined with bedside clinical assessment. Additionally, the intervention of rounding prioritization costs nothing because patients would be rounded on anyway.
尽管 ROX 指数在 COVID-19 患者中的阳性预测值较低,但我们认为嵌入电子健康记录是足够的,因为它将用作四舍五入优先工具,而不是关于是否插管的明确答案。
Although the positive predictive value of ROX index was lower in COVID-19 patients, we felt that it was adequate to embed in the electronic health record because it would be used as a rounding prioritization tool, not a definitive answer about whether to intubate or not.
我们没有探索改变 COVID-19 患者的模型阈值,因为我们倾向于在患者中嵌入一个具有一个阈值的模型。
We did not explore changing the model threshold for COVID-19 patients because we preferred embedding one model with one threshold across patients.
否则,该模型需要电子解释住院早期不准确的诊断。
Otherwise, the model would need to electronically account for diagnoses, which are inaccurate early in hospitalization.
本研究填补了 COVID-19 危险分层的重要空白。
This study fills important gaps in COVID-19 risk stratification.
我们报告了在多个中心接受 HFNC 的显著更大的患者队列 (8-10),这增强了对我们结果的信心。
We report on a substantially larger cohort of patients receiving HFNC across multiple centers (8–10), which bolsters confidence in our findings.
既往研究中的患者和医院数量范围分别为 62-255 例患者和 1-5 家医院 (8-10)。
The range of number of patients and hospitals in previous studies is between 62 and 255 patients and 1–5 hospitals, respectively (8–10).
我们还检查了高度当代的队列,包括在随机图 1 后接受治疗的队列。该图显示了 12 小时时按呼吸频率 - 氧合 (ROX) 风险组列出的出现各种结局的 COVID-19 呼吸衰竭患者百分比。
We also examine a highly contemporary cohort, including those treated after the Randomized Figure 1. This figure shows the percent of patients with COVID-19-related respiratory failure by respiratory rate-oxygenation (ROX) risk group at 12 hours who experience various outcomes.
条形表示以下患者的百分比:1)在高流量插管开始后 24 小时内接受机械通气,2)在住院期间的任何时间接受机械通气,和 3)在医院死亡。
The bars indicate the percent of patients who: 1) received mechanical ventilation within 24 hours of high flow cannular initiation, 2) received mechanical ventilation anytime during hospitalization, and 3) died in the hospital.
COVID-19 治疗评价(RECOVERY)试验确定地塞米松为 COVID-19 肺炎的标准治疗(11)。既往较小的研究包括截至 2020 年 6 月的数据(8-10)。
Evaluation of COVID-19 Therapy (RECOVERY) trial established dexamethasone as standard of care in COVID-19 pneumonia (11). Prior smaller studies included data through June 2020 (8–10).
我们还进行了生存分析,以证实中危和高危 ROX 组与低危 ROX 组相比,有创机械通气或死亡的可能性不同。
We also performed survival analysis to confirm that intermediateand high-risk ROX groups have different likelihoods of invasive mechanical ventilation or death compared with low-risk ROX group.
需要进一步的研究来评估后期时间点的 ROX、ROX 指数各部分的预测能力以及在 COVID-19 中使用无创通气的效用。
Further research is needed to assess ROX at later time points, the predictive capability of each part of the ROX index, and the utility of using noninvasive ventilation in COVID-19.
本研究存在重要的局限性。
This study has important limitations.
呼吸率可能不准确 (12),这可能改变 ROX 值。
Respiratory rate may not be accurate (12), which can alter ROX values.
ROX 中未考虑的因素应指导插管决策,包括患者的呼吸功和分泌物。
Factors not accounted for in ROX should guide decisions to intubate, including patients’ work of breathing and secretions.
因为这是一项验证研究,我们使用了之前用于在 COVID-19 大流行前开发和验证 ROX 的两个阈值。
Because this was a validation study, we used the two thresholds that were previously used to develop and validate ROX prior to the COVID-19 pandemic.
未来研究更严格的阈值可能是有益的。
It may be beneficial in the future to study a stricter threshold.
优势包括其跨越大流行所有浪潮的大型、基于人群的样本,并评估 ROX 风险组的多种结果。
Strengths include its large, population-based sample spanning all waves of the pandemic and evaluating multiple outcomes across ROX risk groups.
结论:COVID-19 开始 HFNC 治疗后 12 小时的 ROX 指数使用小于 3.85 的更严格阈值具有足够的阳性预测值。
CONCLUSIONS ROX index at 12 hours after initiation of HFNC for COVID-19 has adequate positive predictive value using the stricter threshold of less than 3.85.
我们的综合医疗系统已经将 ROX 指数嵌入到电子健康记录中,用作在住院激增期间识别高危患者的四舍五入优先工具。
Our integrated healthcare system has embedded ROX index into the electronic health record to use as a rounding prioritization tool to identify high-risk patients during periods of inpatient surge.
