 危重病期间腹泻
危重病期间腹泻
# 危重病期间腹泻
Diarrhea during critical illness: a multicenter cohort study
危重病期间腹泻:一项多中心队列研究
- Joanna C. Dionne, Lawrence Mbuagbaw Intensive Care Medicine (opens new window) volume 48, pages570–579 (2022)
# 摘要
Purpose To study the incidence, predictors, and outcomes of diarrhea during the stay in the intensive care unit (ICU).
Methods Prospective cohort of consecutive adults in the ICU for > 24 h during a 10-week period across 12 intensive care units (ICUs) internationally. The explored outcomes were: (1) incidence of diarrhea, (2) Clostridioides difficile-associated diarrhea (CDAD); (3) ICU and hospital length of stay (LOS) and mortality in patients with diarrhea. We fit generalized linear models to evaluate the predictors, management, morbidity and mortality associated with diarrhea.
Results Among 1109 patients aged 61.4 (17.5) [mean (standard deviation)] years, 981(88.5%) were medical and 645 (58.2%) were mechanically ventilated. The incidence was 73.8% (818 patients, 73.8%, 95% confidence interval [CI] 71.1–76.6) using the definition of the World Health Organisation (WHO). Incidence varied across definitions (Bristol 53.5%, 95% CI 50.4–56.7; Bliss 37.7%, 95% CI 34.9–40.4). Of 99 patients with diarrhea undergoing CDAD testing, 23 tested positive (2.2% incidence, 95% CI 1.5–3.4). Independent predictors included enteral nutrition (RR 1.23, 95% CI 1.16–1.31, p < 0.001), antibiotic days (RR 1.02, 95% CI 1.02–1.03, p < 0.001), and suppositories (RR 1.14 95% CI 1.06–1.22, p < 0.001). Opiates decreased diarrhea risk (RR 0.76, 95% CI 0.68–0.86, p < 0.001). Diarrhea prompted management modifications (altered enteral nutrition or medications: RR 10.25, 95% CI 5.14–20.45, p < 0.001) or other consequences (fecal management device or CDAD testing: RR 6.16, 95% CI 3.4–11.17, p < 0.001). Diarrhea was associated with a longer time to discharge for ICU or hospital stay, but was not associated with hospital mortality.
Conclusion Diarrhea is common, has several predictors, and prompts changes in patient care, is associated with longer time to discharge but not mortality.
目的 研究在重症监护室(ICU)住院期间腹泻的发生率、预测因素和结果。
方法 在国际上 12 个重症监护室(ICU)中,对连续 10 周内在重症监护室停留 > 24 小时的成人进行前瞻性队列研究。探讨的结果是。(1)腹泻的发生率;(2)艰难梭菌 * 相关的腹泻(CDAD);(3)腹泻患者的 ICU 和住院时间(LOS)以及死亡率。我们拟合广义线性模型来评估与腹泻相关的预测因素、管理、发病率和死亡率。
结果 在 1109 名年龄为 61.4(17.5)[平均(标准差)] 岁的患者中,981 人(88.5%)为内科,645 人(58.2%)为机械通气。采用世界卫生组织(WHO)的定义,发病率为 73.8%(818 名患者,73.8%,95% 置信区间 [CI] 71.1-76.6)。不同定义的发病率有所不同(布里斯托尔 53.5%,95% CI 50.4-56.7;布利斯 37.7%,95% CI 34.9-40.4)。在 99 名接受 CDAD 检测的腹泻患者中,23 人检测结果呈阳性(2.2% 的发生率,95% CI 为 1.5-3.4)。独立的预测因素包括肠内营养(RR 1.23,95% CI 1.16-1.31,p < 0.001),抗生素天数(RR 1.02,95% CI 1.02-1.03,p < 0.001),和栓剂(RR 1.14 95% CI 1.06-1.22,p < 0.001)。阿片类药物降低了腹泻风险(RR 0.76,95% CI 0.68-0.86,p < 0.001)。腹泻促使管理方式的改变(改变肠道营养或药物治疗。RR 10.25, 95% CI 5.14-20.45, p < 0.001)或其他后果(粪便管理装置或 CDAD 测试。RR 6.16,95% CI 3.4-11.17,p < 0.001)。腹泻与出院时间更长的 ICU 或住院时间有关,但与住院死亡率无关。
结论 腹泻很常见,有几个预测因素,并促使病人护理的改变,与出院时间延长有关,但与死亡率无关。
In this study, we demonstrated that diarrhea was common in the intensive care unit, and rarely was Clostridioides difficile the cause. Diarrhea incidence varied based on the definition applied. Diarrhea was associated with longer time to discharge but not increased mortality.
在这项研究中,我们证明了腹泻在重症监护室很常见,而且很少是艰难梭菌 * 的原因。腹泻的发生率根据应用的定义而不同。腹泻与出院时间延长有关,但与死亡率增加无关。
# 序言
The reported incidence of diarrhea during critical illness ranges from 2 to 95% [1 (opens new window), 2 (opens new window)]. Differentiating diarrhea from changes in stool frequency, consistency, and volume that commonly occur during admission to the intensive care unit (ICU) is challenging [3 (opens new window)]. Moreover, wide variation exists regarding what is considered a normal bowel habit in the general population [4 (opens new window)], with definitions ranging from 3 bowel movements per week to 2–3 per day. Thus, there is no universal definition for what constitutes diarrhea in the ICU [5 (opens new window)].
据报道,危重病期间的腹泻发生率在 2% 至 95% 之间 [1 (opens new window), 2 (opens new window)]。将腹泻与入重症监护室(ICU)期间通常发生的大便频率、浓度和体积的变化区分开来具有挑战性 [3 (opens new window)] 。此外,在一般人群中,什么是正常的排便习惯存在很大的差异 [4 (opens new window)],其定义从每周 3 次排便到每天 2-3 次不等。因此,对于什么是 ICU 中的腹泻并没有统一的定义 [5 (opens new window)]。
The World Health Organization (WHO) definition of diarrhea is the passage of 3 or more liquid stools per day [6 (opens new window)], as adopted by the European Society of Intensive Care Medicine Abdominal Problem Working Group [3 (opens new window)]. Perhaps the most recognized stool evaluation instrument in hospitals is the Bristol Stool Chart [7 (opens new window)], which is simple and easily applied at the bedside, composed of descriptive text and a figure depicting each of the seven categories. The Bristol Stool Chart better predicts whole-intestinal transit time than stool frequency [7 (opens new window)], and is used to define diarrhea associated with Clostridioides difficile by the European Society for Clinical Microbiology and Infectious Disease [8 (opens new window), 9 (opens new window)]. The Bliss Stool Classification System has 4 categories with depictions and descriptions for each category. Despite reliability and validity when utilized by health care professionals [10 (opens new window), 11 (opens new window)], this instrument is not widely used in research. Investigations in the ICU setting have employed the Bristol Stool Chart [12 (opens new window)]; however, large studies validating these classification systems in critical illness are lacking.
世界卫生组织(WHO)对腹泻的定义是每天排出 3 次或更多的液体大便 [6 (opens new window)],欧洲重症医学会腹部问题工作组 [3 (opens new window)] 也采用了这个定义。也许医院里最公认的粪便评估工具是布里斯托尔粪便图 [7 (opens new window)],它简单且容易在床边应用,由描述性文字和描述七个类别中每个类别的图组成。布里斯托尔大便图比大便频率更能预测整个肠道的转运时间 [7 (opens new window)],欧洲临床微生物学和传染病协会用它来定义与艰难梭菌有关的腹泻 [8 (opens new window), 9 (opens new window)]。Bliss 粪便分类系统有 4 个类别,每个类别都有描述和说明。尽管卫生保健专业人员使用时具有可靠性和有效性 [10 (opens new window), 11 (opens new window)],但该工具在研究中并未广泛使用。在 ICU 环境中的调查采用了布里斯托尔粪便图 [12 (opens new window)];然而,在危重病中验证这些分类系统的大型研究还缺乏。
Epidemiology of diarrhea in critically ill patients is limited in quality and quantity. A recent systematic review identified 8 observational studies of diarrhea in this setting [5 (opens new window)]. Studies have reported on diarrhea in enterally fed critically ill patients [13 (opens new window)], diarrhea predictors [14 (opens new window), 15 (opens new window)] and manifestations of gastrointestinal failure (e.g., feeding intolerance and ileus) [16 (opens new window)]. Designs included retrospective audits, registry analyses [14 (opens new window)], case–control [16 (opens new window)] and single-center studies[17 (opens new window)]. Another recent systematic review included 12 prospective studies of diarrhea in the ICU [18 (opens new window)]; from the final sample of 12,624 patients, the 1888 patients with diarrhea compared to those without had an associated increased ICU mortality (RR 1.43, 95% CI 1.03, 1.98), an increased length of stay in the ICU (MD 8.08 days, 95% CI 5.85, 10.32) and hospital (MD 9.67 days, 95% CI 2.17 to 17.16) [18 (opens new window)].
危重病人腹泻的流行病学在质量和数量上都很有限。最近的一项系统综述确定了 8 项关于这种情况下腹泻的观察性研究 [5 (opens new window)]。研究报告了肠内喂养的重症患者的腹泻情况 [13 (opens new window)],腹泻预测因素 [14 (opens new window), 15 (opens new window)] 和胃肠功能衰竭的表现(如喂养不耐受和回肠)[16 (opens new window)] 。Designs included retrospective audits, registry analyses [14 (opens new window)], case–control [16 (opens new window)] and single-center studies[17 (opens new window)]. 最近的另一项系统综述包括 12 项关于 ICU 腹泻的前瞻性研究 [18 (opens new window)];从 12,624 名患者的最终样本中,与没有腹泻的患者相比,1888 名患者的 ICU 死亡率(RR 1.43,95% CI 1.03,1.98)增加,在 ICU(MD 8.08 天,95% CI 5.85,10.32)和医院(MD 9.67 天,95% CI 2.17 至 17.16)的停留时间增加 [[18](https://link-springer-com-443.webvpn.cams.cn/article/10.1007/s00134-022-06663-8#ref-CR18)]。
The objectives of this study were to determine the incidence of diarrhea defined using the WHO criteria, including the incidence of Clostridioides difficile-associated diarrhea (CDAD), to compare the incidence and definitions of diarrhea using the Bristol Stool Chart and Bliss Classification System, to identify diarrhea predictors, and to describe the management modifications, consequences, and clinical outcomes associated with diarrhea.
本研究的目的是确定使用 WHO 标准定义的腹泻发生率,包括艰难梭菌 * 相关腹泻(CDAD)的发生率,比较使用布里斯托尔粪便图和 Bliss 分类系统的腹泻发生率和定义,确定腹泻预测因素,并描述与腹泻相关的管理修改、后果和临床结果。
# 方法
The “Diarrhea: Interventions, Consequences and Epidemiology in the Intensive Care Unit” (DICE-ICU) Study is a prospective multicenter cohort study enrolling consecutive patients 18 years of age or older admitted to the ICU for ≥ 24 h. Patients were excluded if they were in ICU for < 24 h; second and subsequent admissions were not considered to avoid non-independent observations. The design is reported elsewhere [19 (opens new window)], including an internal pilot [20 (opens new window)]. Participants were enrolled over a 10-week period in 12 academic and community medical-surgical ICUs in Canada (n = 8), the United States (n = 2), Poland (n = 1), and Saudi Arabia (n = 1). ICUs were enrolled serially, each determining its own 10-week study period from July 2014–August 2019 (internal pilot 2014–2015, main cohort 2016–2019). Patients were followed daily in the ICU until discharge, then hospital vital status and length of stay was documented, censored at 1 year. DICE-ICU was approved by the research ethics board at each center with a waiver of informed consent except for 1 center which mandated a priori written consent. DICE is reported per STROBE guidelines [21 (opens new window)].
腹泻:重症监护室的干预、后果和流行病学 "(DICE-ICU)研究是一项前瞻性的多中心队列研究,连续招募 18 岁或以上入住重症监护室≥24 小时的患者,如果患者在重症监护室的时间 < 24 小时,则被排除;为避免非独立观察,不考虑第二次和后续的入院。该设计已在其他地方报告 [19 (opens new window)],包括一个内部试点 [20 (opens new window)]。参与者在加拿大(n=8)、美国(n=2)、波兰(n=1)和沙特阿拉伯(n=1)的 12 个学术和社区内外科 ICU 中进行了为期 10 周的登记。ICU 连续入选,每个 ICU 确定自己的 10 周研究期,从 2014 年 7 月 - 2019 年 8 月(2014-2015 年内部试点,2016-2019 年主要队列)。在 ICU 每天对患者进行随访,直到出院,然后记录医院的生命状态和住院时间,1 年后进行删减。DICE-ICU 得到了每个中心的研究伦理委员会的批准,除了 1 个中心规定事先要有书面同意外,其他中心都放弃了知情同意。DICE 的报告是根据 STROBE 指南 [21 (opens new window)]。
The research team trained bedside nurses [19 (opens new window)] to track the number and character of each stool daily. The reference standard and primary outcome were the WHO definition of at least 3 liquid bowel movements per day [6 (opens new window)]; we also used the Bristol Stool Chart Score of 6 or 7 [7 (opens new window)] and Bliss Stool Classification System score of 4 [10 (opens new window)] as secondary diarrhea definitions. We used patients’ first episode of diarrhea after their admission to ICU as the index case. We defined confirmed CDAD as positive microbiology testing with the presence of diarrhea based on the WHO definition.
Research staff collected baseline patient characteristics (i.e., age, sex, pre-hospital comorbidities, Acute Physiology and Chronic Health Evaluation II (APACHE II) score [22 (opens new window)], admission diagnosis and pre-existing gastrointestinal conditions (i.e., inflammatory bowel disease, Celiac disease, short bowel syndrome, prior bowel resection, chronic pancreatitis, and gastroparesis, CDAD, ileostomy or colostomy). Research staff collected daily life support (i.e., invasive mechanical ventilation, vasopressors, renal replacement therapy), laboratory values, enteral nutrition (i.e., formulation, route, volume, and interruptions), medications known to influence the risk of diarrhea, and management modifications and consequence of diarrhea. CDAD testing was performed at the physician’s discretion. Mortality and length of ICU and hospital stay were documented, censored at 1 year.
Data were validated by research staff and the principal investigator (JCD) at McMaster University’s Methods Center.
研究小组对床边护士进行了培训 [19 (opens new window)],让她们每天跟踪每一次大便的数量和特征。参考标准和主要结果是 WHO 定义的每天至少 3 次液体排便 [6 (opens new window)];我们还使用布里斯托尔大便图表得分 6 或 7 [7 (opens new window)] 和 Bliss 大便分类系统得分 4 [10 (opens new window)] 作为次要腹泻定义。我们将患者入院后的第一次腹泻作为索引病例。根据 WHO 的定义,我们将确诊的 CDAD 定义为微生物学检测呈阳性并有腹泻出现。
研究人员收集了患者的基线特征(即年龄、性别、院前合并症、急性生理和慢性健康评估 II(APACHE II)评分 [22 (opens new window)]、入院诊断和先前存在的胃肠道疾病(即炎症性肠病、乳糜泻、短肠综合征、先前肠切除术、慢性胰腺炎和胃痉挛、CDAD、回肠造口或结肠造口)。研究人员收集了日常生活支持(即有创机械通气、血管抑制剂、肾脏替代治疗)、实验室数值、肠内营养(即配方、途径、容量和中断)、已知影响腹泻风险的药物,以及管理修改和腹泻的后果。CDAD 测试是由医生决定进行的。死亡率、ICU 和住院时间都有记录,1 年后进行删减。
数据由麦克马斯特大学方法中心的研究人员和主要研究人员(JCD)进行验证。
This work was supported by peer-review grants from Hamilton Regional Medical Associates, McMaster University Department of Medicine, Physicians Services Incorporated of Ontario, and the Canadian Association of Gastroenterology which had no role in the design, analysis or interpretation of data or manuscript.
这项工作得到了汉密尔顿地区医疗协会、麦克马斯特大学医学部、安大略省医生服务有限公司和加拿大胃肠病学协会的同行评审资助,这些机构在数据的设计、分析或解释或手稿中没有发挥作用。
The methodology and statistical analysis plan were published [19 (opens new window)]. Briefly, our sample size was derived by two approaches: (1) the rule of thumb based on independent predictors and number of events per degree of freedom and (2) the DICE internal pilot primary objectives. Baseline characteristics were analysed descriptively, reported as counts (percent), mean (standard deviation) or median (quartile 1, quartile 3) as appropriate.
The incidence of diarrhea was the proportion of participants who developed diarrhea on day 1 or later in the ICU (WHO as the primary definition), and the Bristol and Bliss scores (secondary definitions). We also calculated the incidence rate (number of new cases of diarrhea divided by person-time at risk in the ICU). The prevalence of CDAD was calculated as the proportion of patients with CDAD upon ICU admission and the number of cases acquired in ICU. The incidence of CDAD was calculated as the proportion of patients with diarrhea subsequently testing positive during their ICU admission (new cases).
Using the kappa statistic, we calculated agreement between the WHO, Bliss and Bristol definitions.
方法和统计分析计划已发表 [19 (opens new window)]。简而言之,我们的样本量是通过两种方法得出的:(1)基于独立预测因素和每个自由度的事件数的经验法则;(2)DICE 内部试点的主要目标。对基线特征进行描述性分析,酌情以计数(百分比)、平均值(标准差)或中位数(四分位数 1,四分位数 3)报告。
腹泻的发生率是指在 ICU 第 1 天或以后发生腹泻的参与者的比例(WHO 为主要定义),以及布里斯托尔和 Bliss 的评分(次要定义)。我们还计算了发病率(新的腹泻病例数除以在 ICU 的风险人时)。CDAD 的患病率是以入院时患有 CDAD 的患者比例和在 ICU 获得的病例数来计算。CDAD 的发病率是指在 ICU 入院时腹泻患者中检测出阳性的比例(新病例)。
使用卡帕统计学,我们计算了 WHO、Bliss 和 Bristol 定义之间的一致性。
We deviated from the previously published statistical plan [19 (opens new window)]. Odds ratios (OR) were the initial estimate of effect planned to be reported in DICE-ICU; however, given the frequency of diarrhea being common rather than uncommon, an RR was determined to be a better estimate of effect (Statistical Appendix).
For all adjusted analyses [23 (opens new window)], we used generalized linear models. We specified a log link, a normal distribution (to estimate adjusted risk ratios) with clustered robust standard errors to account for potential clustering within centers. Model comparison was facilitated using Akaike information criteria (AIC). Potential diarrhea predictors (per the WHO definition [6 (opens new window)])were determined based on previous studies identifying antibiotics, antifungals, suppository, pro-kinetics, CDAD, and enteral nutrition [2 (opens new window), 13 (opens new window), 14 (opens new window)], further refined during the DICE pilot study [20 (opens new window)]. The following covariates were entered as a block: baseline factors, such as age (years), sex (female/male), APACHE II score (0–71); exposures in the ICU prior to diarrhea (enteral nutrition (yes/no), and medications [opiates, motility agents, sorbitol, acid suppressants (yes/no), total number of antibiotics (ratio) and the number of days on antibiotics (ratio), and chemotherapy (yes/no)]. We examined the events prior to diarrhea (predictors of diarrhea) separately from the events after diarrhea (consequences of diarrhea). We also analyzed differences in diarrhea predictors for the Bristol Stool Chart and Bliss Stool Classification. We first examined univariate associations. Only predictors that were statistically significant at the p < 0.05 threshold were included in the multivariable models.
我们偏离了以前公布的统计计划 [19 (opens new window)]。比率(OR)是 DICE-ICU 计划报告的最初效果估计;然而,鉴于腹泻的频率是常见的而不是不常见的,RR 被确定为效果的更好估计(统计学附录)。
对于所有调整后的分析 [23 (opens new window)],我们使用广义线性模型。我们指定了一个对数联系,一个正态分布(以估计调整后的风险比),并有分组的稳健标准误差,以考虑到中心内的潜在集群。使用 Akaike 信息标准(AIC)促进了模型的比较。潜在的腹泻预测因素(根据 WHO 的定义 [6 (opens new window)])是根据以前的研究确定的,包括抗生素、抗真菌药、栓剂、促动力、CDAD 和肠道营养 [2 (opens new window), 13 (opens new window), 14 (opens new window)],在 DICE 试点研究中进一步完善 [20 (opens new window)]。以下协变量被作为一个区块输入:基线因素,如年龄(岁)、性别(女 / 男)、APACHE II 评分(0-71);腹泻前在 ICU 的暴露(肠内营养(是 / 否),以及药物 [阿片类药物、促动剂、山梨醇、抑酸剂(是 / 否)、抗生素总数(比率)和使用抗生素的天数(比率),以及化疗(是 / 否)] 。我们分别研究了腹泻前的事件(腹泻的预测因素)和腹泻后的事件(腹泻的后果)。我们还分析了布里斯托尔大便图和 Bliss 大便分类的腹泻预测因素的差异。我们首先检查了单变量的关联。只有在 p<0.05 阈值下有统计学意义的预测因素被纳入多变量模型。
We fitted similar models to examine the management modifications and consequences of diarrhea adjusting for age, sex, and APACHE II score. Management modifications were any of altered enteral nutrition (i.e., feeds held or decreased, formula changed), stool softener or pro-kinetic held, or anti-diarrheal agent administered. Management consequences were either fecal management device insertion or CDAD testing. These were all entered as binary (yes/no).
We used the Wilcoxon rank-sum test to compare length of stay in the ICU and hospital between patients with and without diarrhea. To determine the impact of diarrhea on death, ICU discharge and hospital discharge, we attempted to fit Cox proportional hazards models. For the outcome of death at any time, we assumed that discharge was a competing risk, and modelled both failures (death) and competing risk events (discharge). For the outcomes of ICU discharge and hospital discharge, we considered death as a competing risk. In the latter two models, the proportional hazards assumption was not met, so we compared six parametric model distributions (Weibull, Lognormal, Loglogistic, Gompertz, Exponential and Generalized Gamma) and reported the one with the lowest AIC score. All the models were adjusted for age, sex, APACHE score and the standard errors were adjusted for clustering within centres. Hazard ratios (HR), 95% confidence intervals (CI) and p values are reported. Imputation methods were planned a priori in the case of significant missing data [19 (opens new window)]. All analyses were performed using Stata (StataCorp, Release 16, 2019, College Station; TX) [24 (opens new window)].
我们建立了类似的模型来研究管理修改和腹泻的后果,调整了年龄、性别和 APACHE II 评分。管理调整是指改变肠道营养(即暂停或减少喂食,改变配方),使用大便软化剂或促动力剂,或使用抗腹泻药。管理后果是插入粪便管理装置或进行 CDAD 测试。这些都是以二进制(是 / 否)的形式输入。
我们使用 Wilcoxon 秩和检验来比较有腹泻和无腹泻患者在 ICU 和医院的停留时间。为了确定腹泻对死亡、ICU 出院和出院的影响,我们试图拟合 Cox 比例危害模型。对于任何时候的死亡结果,我们假设出院是一种竞争性风险,并对失败(死亡)和竞争性风险事件(出院)进行建模。对于 ICU 出院和出院的结果,我们认为死亡是一种竞争性风险。在后两个模型中,不符合比例危害假设,因此我们比较了六个参数模型分布(Weibull、Lognormal、Loglogistic、Gompertz、Exponential 和 Generalized Gamma),并报告了 AIC 得分最低的一个。所有的模型都根据年龄、性别、APACHE 评分进行了调整,标准误差也根据中心内的聚类情况进行了调整。报告了危险比(HR)、95% 置信区间(CI)和 P 值。在数据严重缺失的情况下,事先计划了代偿方法 [19 (opens new window)]。所有分析均使用 Stata(StataCorp,Release 16,2019,College Station; TX)[24 (opens new window)] 进行。
# 结果
From June 2014 to August 2019, 1114 patients were enrolled at 12 academic and community ICUs in Canada, the United States, Poland and Saudi Arabia (Fig. 1 (opens new window)), 1109 of whom were included in this study. The mean (standard deviation) age was 61.4 (17.5) years, APACHE II score was 18.8 (8), and 591 (53.2%) were mechanically ventilated at baseline on study day 1 (Table 1 (opens new window)). Most patients were medical (981, 88.5%). Diarrhea-related comorbidities at ICU admission included colectomy or ileostomy (2.4%), and inflammatory bowel disease (0.1%). Our dataset was complete with very few missing data (< 1%), and the imputation was not required. For main outcomes, patients with complete data were used.
从 2014 年 6 月到 2019 年 8 月,加拿大、美国、波兰和沙特阿拉伯的 12 个学术和社区 ICU 共招募了 1114 名患者(图 1 (opens new window)),其中 1109 人被纳入本研究中。平均(标准差)年龄为 61.4(17.5)岁,APACHE II 评分为 18.8(8)分,591(53.2%)人在研究第 1 天的基线上使用机械呼吸(表 1 (opens new window))。大多数患者是内科(981,88.5%)。入院时与腹泻有关的合并症包括结肠切除术或回肠造口术(2.4%),以及炎症性肠病(0.1%)。我们的数据集是完整的,缺失的数据非常少(<1%),不需要进行归因处理。对于主要结果,我们使用了具有完整数据的患者。
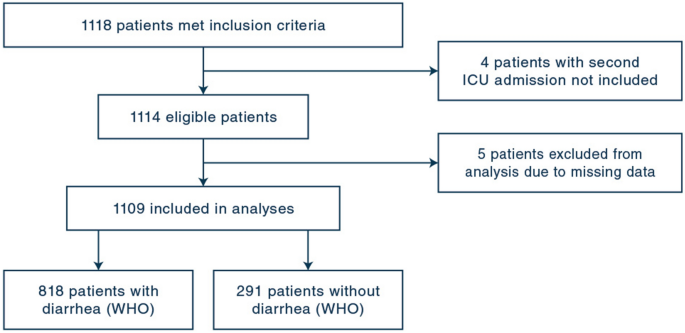
# 图. 1
Flow Diagram for DICE-ICU Study. Flow diagram of patients enrolled in the DICE-ICU Study
DICE-ICU 研究的流程图。DICE-ICU 研究入选患者的流程图
# 表 1 基线特征
| Characteristics | Total Cohort ( n = 1109) | Diarrhea ( n = 818) | No Diarrhea ( n = 291) |
|---|---|---|---|
| Sex (female), n (%) | 489 (44.1) | 372 (45.5) | 117 (40.2) |
| Age, mean (SD) | 61.4 (17.5) | 61.8 (17.2) | 60.3 (18.3) |
| APACHE II score, mean (SD) a | 18.8 (7.98) | 19.1 (7.8) | 17.8 (8.5) |
| Type of patient, n (%) b | |||
| Medical | 981 (88.5) | 731 (89.9) | 250 (86.5) |
| Surgical | 59 (5.3) | 38 (4.7) | 21 (7.3) |
| Trauma | 62 (5.6) | 44 (5.4) | 18 (6.2) |
| Admitting Diagnosis, n (%) c | |||
| Cardiovascular | 140 (12.6) | 95 (11.7) | 45 (15.6) |
| Respiratory | 272 (24.5) | 214 (26.3) | 58 (20.1) |
| Gastrointestinal | 161 (14.5) | 119 (14.6) | 42 (14.5) |
| Neurologic | 137 (12.4) | 98 (12.1) | 39 (13.5) |
| Sepsis | 117 (10.6) | 95 (11.7) | 22 (7.6) |
| Trauma | 62 (5.6) | 44 (5.4) | 18 (6.2) |
| Metabolic | 86 (7.8) | 55 (6.8) | 31 (10.7) |
| Hematologic | 10 (0.9) | 9 (1.1) | 1 (0.3) |
| Renal | 30 (2.7) | 24 (3) | 6 (2.1) |
| Gynecologic | 2 (0.2) | 2 (0.2) | 0 (0) |
| Orthopaedic surgery | 14 (1.3) | 8 (1) | 6 (2.1) |
| Cardiovascular surgery | 6 (0.5) | 2 (0.2) | 4 (1.4) |
| Other medical | 28 (2.5) | 22 (2.7) | 6 (2.1) |
| Other surgical | 37 (3.3) | 26 (3.2) | 11 (3.8) |
| Location Prior to ICU, n (%) d | |||
| Emergency room | 451 (40.7) | 327 (40) | 124 (42.6) |
| Hospital ward | 266 (24) | 221 (27) | 45 (15.5) |
| OR/Recovery room | 221 (19.9) | 129 (15.8) | 92 (31.6) |
| Other | 46 (4.1) | 42 (5.1) | 4 (1.4) |
| ICU (other hospital) | 45 (4.1) | 38 (4.6) | 7 (2.4) |
| Emergency (other hospital) | 58 (5.2) | 42 (5.1) | 16 (5.5) |
| Ward (other hospital) | 21 (1.9) | 18 (2.2) | 3 (1) |
| Relevant comorbid conditions, n (%) | |||
| Celiac disease e | 2 (0.1) | 1 (0.1) | 1 (0.3) |
| Irritable bowel | 6 (0.5) | 5 (0.6) | 1 (0.3) |
| Diabetes | 318 (28.7) | 229 (28) | 89 (30.6) |
| Prior bowel resection surgery | 30 (2.7) | 25 (3.1) | 5 (1.7) |
| Inflammatory bowel disease (Crohn disease, ulcerative colitis) | 24 (2.2) | 22 (2.7) | 2 (0.7) |
| Colectomy/ileostomy | 27 (2.4) | 21 (2.6) | 6 (2.1) |
| Chronic pancreatitis | 10 (0.9) | 8 (1) | 2 (0.7) |
| Current Clostridium Difficile infection | 11 (.1) | 9 (1.1) | 2 (0.7) |
| Gastroparesis | 7 (0.6) | 6 (0.7) | 1 (0.3) |
| Study Day 1, n (%) | |||
| Invasive mechanical ventilation f | 591 (53.2) | 455 (55.9) | 136 (46.7) |
| Inotropes or vasopressors g | 405 (36.5) | 304 (37.3) | 101 (34.9) |
| Dialysis/renal replacement h | 79 (7.1) | 59 (7.3) | 20 (6.9) |
- In this table we present baseline characteristics of 1,109 critically ill patients. Surgical patients were defined according to Canadian Critical Care Trials group definition
- SD standard deviation, APACHE Acute Physiology and Chronic Health Evaluation
- a8 missing
- b7 missing
- c7 missing
- d9 missing
- e1 missing
- f4 missing
- g6 missing
- h6 missing
| 特征 | 总队列 (n = 1109) | 腹泻 (n = 818) | 无腹泻 (n = 291) |
|---|---|---|---|
| 性别(女性),n(%)。 | 489 (44.1) | 372 (45.5) | 117 (40.2) |
| 年龄,平均 (SD) | 61.4 (17.5) | 61.8 (17.2) | 60.3 (18.3) |
| APACHE II 评分,平均(SD)a | 18.8 (7.98) | 19.1 (7.8) | 17.8 (8.5) |
| 病人类型,n (%) b | |||
| 内科 | 981 (88.5) | 731 (89.9) | 250 (86.5) |
| 外科 | 59 (5.3) | 38 (4.7) | 21 (7.3) |
| 创伤 | 62 (5.6) | 44 (5.4) | 18 (6.2) |
| 入院诊断,n (%) c | |||
| 心血管系统 | 140 (12.6) | 95 (11.7) | 45 (15.6) |
| 呼吸系统 | 272 (24.5) | 214 (26.3) | 58 (20.1) |
| 胃肠道 | 161 (14.5) | 119 (14.6) | 42 (14.5) |
| 神经系统 | 137 (12.4) | 98 (12.1) | 39 (13.5) |
| 败血症 | 117 (10.6) | 95 (11.7) | 22 (7.6) |
| 创伤 | 62 (5.6) | 44 (5.4) | 18 (6.2) |
| 代谢性疾病 | 86 (7.8) | 55 (6.8) | 31 (10.7) |
| 血液学 | 10 (0.9) | 9 (1.1) | 1 (0.3) |
| 肾脏 | 30 (2.7) | 24 (3) | 6 (2.1) |
| 妇科 | 2 (0.2) | 2 (0.2) | 0 (0) |
| 骨科手术 | 14 (1.3) | 8 (1) | 6 (2.1) |
| 心血管外科 | 6 (0.5) | 2 (0.2) | 4 (1.4) |
| 其他内科 | 28 (2.5) | 22 (2.7) | 6 (2.1) |
| 其他外科手术 | 37 (3.3) | 26 (3.2) | 11 (3.8) |
| 进入 ICU 前的地点,n (%) d | |||
| 急诊室 | 451 (40.7) | 327 (40) | 124 (42.6) |
| 医院病房 | 266 (24) | 221 (27) | 45 (15.5) |
| 手术室 / 恢复室 | 221 (19.9) | 129 (15.8) | 92 (31.6) |
| 其他 | 46 (4.1) | 42 (5.1) | 4 (1.4) |
| 重症监护室 (其他医院) | 45 (4.1) | 38 (4.6) | 7 (2.4) |
| 急诊 (其他医院) | 58 (5.2) | 42 (5.1) | 16 (5.5) |
| 病房(其他医院) | 21 (1.9) | 18 (2.2) | 3 (1) |
| 相关合并症,n (%) | |||
| 糜烂性疾病 | 2 (0.1) | 1 (0.1) | 1 (0.3) |
| 肠易激综合征 | 6 (0.5) | 5 (0.6) | 1 (0.3) |
| 糖尿病 | 318 (28.7) | 229 (28) | 89 (30.6) |
| 以前做过肠切除手术 | 30 (2.7) | 25 (3.1) | 5 (1.7) |
| 炎症性肠病(克罗恩病、溃疡性结肠炎)。 | 24 (2.2) | 22 (2.7) | 2 (0.7) |
| 结肠切除术 / 结肠造口术 | 27 (2.4) | 21 (2.6) | 6 (2.1) |
| 慢性胰腺炎 | 10 (0.9) | 8 (1) | 2 (0.7) |
| 目前有梭状芽孢杆菌感染 | 11 (.1) | 9 (1.1) | 2 (0.7) |
| 胃痉挛 | 7 (0.6) | 6 (0.7) | 1 (0.3) |
| 研究第 1 天,n (%) | |||
| 侵入性机械通气 f | 591 (53.2) | 455 (55.9) | 136 (46.7) |
| 肌注或血管抑制剂 g | 405 (36.5) | 304 (37.3) | 101 (34.9) |
| 透析 / 肾脏替代疗法 | 79 (7.1) | 59 (7.3) | 20 (6.9) |
- 在这个表中,我们介绍了 1109 名危重病人的基线特征。外科病人的定义是根据加拿大危重病试验组的定义。
- SD 标准差,APACHE 急性生理学和慢性健康评估
- a8 缺失
- b7 缺失
- c7 缺失
- d9 缺少
- e1 缺少
- f4 不适用
- g6 不适用
- 缺少 h6
# 腹泻的发生率
Incidence of diarrhea
Based on the WHO definition, 818 of 1109 patients developed diarrhea, for an incidence of 73.8% (95% CI 71.1–76.6); the median (quartile 1–quartile 3) time to diarrhea onset was 2 (1–4) days, for an incidence rate of 224.6/1000 person-days (95% CI 209.5–240.6). The incidence of diarrhea was 53.5% (95% CI 50.4–56.7) using the Bristol Stool Chart and 37.7% (95% CI 34.9–40.4) using the Bliss Stool Classification System. The incidence differed across centers, with a low of 53% and high of 94% (Appendix Table 1).
根据 WHO 的定义,1109 名患者中有 818 人发生了腹泻,发病率为 73.8%(95% CI 71.1-76.6);腹泻发病时间的中位数(四分位数 1 - 四分位数 3)为 2(1-4)天,发病率为 224.6/1000 人天(95% CI 209.5-240.6)。使用布里斯托尔粪便图,腹泻的发生率为 53.5%(95% CI 为 50.4-56.7),使用 Bliss 粪便分类系统,发生率为 37.7%(95% CI 为 34.9-40.4)。各个中心的发病率不同,最低为 53%,最高为 94%(附录表 1)。
The prevalence of CDAD (Appendix Fig. 1) in the ICU, including pre-ICU CDAD and ICU-acquired CDAD, was 85/1109 (7.7%, 95% CI 6.2–9.4). A total of 62/1109 (5.5%) had CDAD at admission to ICU. However, among 99 patients tested for CDAD, only 23 were positive (CDAD incidence in the ICU 2.2%, 95% CI 1.5–3.4).
ICU 中 CDAD(附录图 1)的发病率,包括 ICU 前 CDAD 和 ICU 获得的 CDAD,为 85/1109(7.7%,95% CI 为 6.2-9.4)。共有 62/1109(5.5%)在进入 ICU 时有 CDAD。然而,在 99 名接受 CDAD 检测的患者中,只有 23 人呈阳性(CDAD 在 ICU 的发病率为 2.2%,95% CI 为 1.5-3.4)。
# 腹泻定义的比较:WHO、Bristol 和 Bliss
Comparison of the definitions of diarrhea: WHO, Bristol and Bliss
Compared with the WHO definition of diarrhea, agreement with a Bristol Stool Chart score of 6 or 7 was moderate (Kappa = 0.51, 95% CI 0.46–0.55, p < 0.001) and with a Bliss score of 4 was fair (Kappa = 0.31, 95% CI 0.27–0.35, p < 0.001). The pooled agreement across 3 definitions was fair (Kappa = 0.39, 95% CI 0.36–0.42, p < 0.001) (Appendix Fig. 2). The WHO definition of diarrhea identifies more patients with diarrhea and is the definition used for this study.
与 WHO 的腹泻定义相比,与布里斯托尔粪便表 6 或 7 分的一致性为中等(Kappa = 0.51,95% CI 0.46-0.55,p < 0.001),与 Bliss 4 分的一致性为一般(Kappa = 0.31,95% CI 0.27-0.35,p < 0.001)。3 种定义的集合一致性尚可(Kappa = 0.39,95% CI 0.36-0.42,p < 0.001)(附录图 2)。世卫组织的腹泻定义可识别更多的腹泻患者,是本研究使用的定义。
# 腹泻的预测因素
Predictors of diarrhea
Independent diarrhea predictors (WHO definition) included enteral nutrition (RR 1.23, 95% CI 1.16–1.31, p < 0.001), number of antibiotic days (RR 1.02, 95% CI 1.02–1.03, p < 0.001) and suppository use (RR 1.14 95% CI 1.06–1.22, p < 0.001) (Table 2 (opens new window)). Opiates (RR 0.76, 95% CI 0.68–0.86, p < 0.001) were associated with decreased diarrhea.
独立的腹泻预测因素(WHO 定义)包括肠内营养(RR 1.23,95% CI 1.16-1.31,p<0.001),抗生素天数(RR 1.02,95% CI 1.02-1.03,p<0.001)和栓剂使用(RR 1.14 95% CI 1.06-1.22,p<0.001)(表[2](https://link-springer-com-443.webvpn.cams.cn/article/10.1007/s00134-022-06663-8#Tab2))。阿片类药物(RR 0.76,95% CI 0.68-0.86,p < 0.001)与腹泻的减少有关。
# 表 2:腹泻的预测因素
| Model | Univariate | Multivariable | Multivariable (Reduced) | |||
|---|---|---|---|---|---|---|
| Covariates | Crude RR (95% CI) | P-value | Adjusted RR (95%CI) | P -value | Adjusted RR (95%CI) | P-value |
| Sex (female) | 1.00 (1.00–1.00) | 0.243 | 0.94 (0.89–1.00) | 0.066 | ||
| Age (years) | 0.95 (0.86–1.95) | 0.276 | 1.00 (1.00–1.01) | 0.101 | ||
| APACHE II score (0–71) | 1.00 (1.00–1.01) | 0.096 | 1.00 (0.99–1.00) | 0.173 | ||
| Opiates (yes)* | 0.92 (0.82–1.03) | 0.139 | 0.76 (0.67–0.86) | <0.001 | 0.76 (0.68–0.86) | <0.001 |
| Chemotherapy (yes)* | 1.07 (0.077–1.48) | 0.677 | 1.05 (0.91–1.20) | 0.509 | ||
| Antibiotics (total no.) | 1.08 (1.05–1.11) | <0.001 | 1.03 (1.00–1.05) | 0.030 | 1.03 (1.00–1.06) | 0.097 |
| Antibiotic days (days) | 1.04 (1.03–1.05) | <0.001 | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.02–1.03) | <0.001 |
| Motility Agent (yes)* | 1.19 (1.11–1.28) | <0.001 | 1.04 (0.98–1.10) | 0.200 | ||
| Sorbitol (yes)* | 1.08 (0.97–1.20) | 0.162 | 1.06 (0.96–1.17) | 0.225 | ||
| Suppository (yes)* | 1.26 (1.15–1.37) | <0.001 | 1.13 (1.06–1.19) | <0.001 | 1.14 (1.06–1.22) | <0.001 |
| Enteral Nutrition (yes)* | 1.37 (1.26–1.50) | <0.001 | 1.23 (1.16–1.31) | <0.001 | 1.23 (1.16–1.31) | <0.001 |
| Acid Suppressants (yes) | 1.15 (1.03–1.30) | 0.017 | 1.08 (0.94–1.23) | 0.294 | ||
| Gastrointestinal comorbidities (yes)* ** | 1.09 (0.95–1.24) | 0.225 | 0.98 (0.93–1.04) | 0.507 | ||
| AIC | NA | 0.982 | 0.982 |
- In this table we present independent predictors for diarrhea (WHO definition) using a generalized linear model, adjusting for age, sex, APACHE II Score, opiates, chemotherapy, number of antibiotics, antibiotic days, motility agent, sorbitol, suppository, enteral nutrition, acid suppressants, gastrointestinal comorbidities, and center. Total number of antibiotics reflects the number of unique antibiotics that a patient received
- RR= Risk Ratio.CI=confidence interval. APACHE=Acute Physiology and Chronic Health Evaluation, AIC= Akaike Information Criterion
- *Reference category is “no
- **Celiac disease, Prior bowel resection surgery, Inflammatory bowel disease (Crohn disease, ulcerative colitis), Colectomy/Ileostomy, Chronic Pancreatitis, Gastroparesis, Diabetes
| 模型 | 单变量 | 多变量 | 多变量 (减少) | |||
|---|---|---|---|---|---|---|
| 协变量 | 粗略 RR (95% CI) | P 值 | 调整后的 RR (95% CI) | P - 值 | 调整后的 RR (95% CI) | P - 值 |
| 性别 (女) | 1.00 (1.00-1.00) | 0.243 | 0.94 (0.89-1.00) | 0.066 | ||
| 年龄 (岁) | 0.95 (0.86-1.95) | 0.276 | 1.00 (1.00-1.01) | 0.101 | ||
| APACHE II 评分 (0-71) | 1.00 (1.00-1.01) | 0.096 | 1.00 (0.99-1.00) | 0.173 | ||
| 阿片类药物(是)* | 0.92 (0.82-1.03) | 0.139 | 0.76 (0.67-0.86) | <0.001 | 0.76 (0.68-0.86) | <0.001 |
| 化疗(是)* | 1.07 (0.077-1.48) | 0.677 | 1.05 (0.91-1.20) | 0.509 | ||
| 抗生素(总数量) | 1.08 (1.05-1.11) | <0.001 | 1.03 (1.00-1.05) | 0.030 | 1.03 (1.00-1.06) | 0.097 |
| 抗生素使用天数(天) | 1.04 (1.03-1.05) | <0.001 | 1.02 (1.01-1.03) | <0.001 | 1.02 (1.02-1.03) | <0.001 |
| 动情剂(是)* | 1.19 (1.11-1.28) | <0.001 | 1.04 (0.98-1.10) | 0.200 | ||
| 山梨醇(是)* | 1.08 (0.97-1.20) | 0.162 | 1.06 (0.96-1.17) | 0.225 | ||
| 栓剂(是)* | 1.26 (1.15-1.37) | <0.001 | 1.13 (1.06-1.19) | <0.001 | 1.14 (1.06-1.22) | <0.001 |
| 肠内营养(是)* | 1.37 (1.26-1.50) | <0.001 | 1.23 (1.16-1.31) | <0.001 | 1.23 (1.16-1.31) | <0.001 |
| 抑酸剂(是) | 1.15 (1.03-1.30) | 0.017 | 1.08 (0.94-1.23) | 0.294 | ||
| 胃肠道合并症(是)* ** | 1.09 (0.95-1.24) | 0.225 | 0.98 (0.93-1.04) | 0.507 | ||
| AIC | 不适用 | 0.982 | 0.982 |
- 在本表中,我们使用广义线性模型,调整了年龄、性别、APACHE II 评分、阿片类药物、化疗、抗生素数量、抗生素天数、促动剂、山梨醇、栓剂、肠内营养、抑酸剂、胃肠道合并症和中心,提出了腹泻的独立预测因素(WHO 定义)。抗生素总数反映了患者接受的独特的抗生素数量。
- RR = 风险比。CI = 置信区间。APACHE = 急性生理和慢性健康评估,AIC=Akaike 信息判据。
- * 参考类别为 " 无
- ** 乳糜泻、先前的肠切除手术、炎症性肠病(克罗恩病、溃疡性结肠炎)、结肠切除术 / 回肠切除术、慢性胰腺炎、胃痉挛、糖尿病
Predictors for diarrhea using the Bristol Stool Chart definition were similar to the WHO definition (Appendix Table 2A, B); however, two additional predictors were age (RR 1.00, 95% CI 1.00–1.01, p = 0.034) and total number of antibiotics (RR 1.05, 95% CI 1.01–1.10, p = 0.019). Considering the Bliss Stool Classification, diarrhea predictors were similar to the WHO and Bristol definitions, with the addition of female sex (RR 1.11, 95% CI 1.01–1.22, p = 0.030) and acid suppressants (RR 1.66, 95% CI 1.15–2.40, p = 0.007) (Appendix Table 2A, B).
使用布里斯托尔大便图表定义的腹泻预测因素与 WHO 定义相似(附录表 2A,B);然而,另外两个预测因素是年龄(RR 1.00,95% CI 1.00-1.01,p = 0.034)和抗生素总数(RR 1.05,95% CI 1.01-1.10,p = 0.019)。考虑到 Bliss 粪便分类,腹泻预测因素与 WHO 和布里斯托尔的定义相似,但增加了女性性别(RR 1.11,95% CI 1.01-1.22,p = 0.030)和抑酸剂(RR 1.66,95% CI 1.15-2.40,p = 0.007)(附录表 2A, B)。
A post hoc analysis of enteral nutrition composition on the impact of diarrhea in this cohort, after adjustment for antibiotics and suppositories, demonstrated that high osmolarity EN (RR 1.14, 95% CI 1.08–1.20, p < 0.001) and high-fiber enteral nutrition (RR 1.11, 95% CI 1.11–1.17, p < 0.001) were feeding compositional features associated with diarrhea (Appendix Table 3).
在调整了抗生素和栓剂后,对该队列中肠道营养成分对腹泻影响的事后分析表明,高渗透压 EN(RR 1.14,95% CI 1.08-1.20,p <0.001)和高纤维肠道营养(RR 1.11,95% CI 1.11-1.17,p <0.001)是与腹泻相关的喂养成分特征(附录表 3)。
We re-examined age in 5-, 10- and 20-year increments. The differences were too small to see, even when reported to two decimal places. We also analyzed 5-point increments of the APACHE score and the differences were still very small. For example, a 10-year increase in age corresponds to a 1% increase in diarrhea and a 5-point increase in APACHE score corresponds to a 1% increase in risk of diarrhea.
我们以 5 年、10 年和 20 年为单位重新审查了年龄。即使报告到小数点后两位,差异也太小了,看不出来。我们还分析了 APACHE 评分的 5 分增量,差异仍然非常小。例如,年龄增加 10 年相当于腹泻增加 1%,APACHE 评分增加 5 分相当于腹泻风险增加 1%。
# 腹泻管理的调整与预后
Management modifications and consequences of diarrhea
The most frequent management modification prompted by diarrhea was holding a stool softener, and most frequent management consequence was ordering a CDI test (Table 3 (opens new window)). After adjusting for age, sex, center and APACHE II score, diarrhea was associated with at least at least one management modification: discontinuing stool softener or pro-kinetic (RR 10.25, 95% CI 5.14–20.45, p < 0.001) and fecal management devices (rectal bag applied or rectal tube inserted) or C. difficile testing (RR 6.16, 95% CI 3.4–11.17, p < 0.001).
腹泻促使的最常见的管理修改是持有大便软化剂,最常见的管理后果是下令进行 CDI 检测(表 3 (opens new window))。在调整了年龄、性别、中心和 APACHE II 评分后,腹泻与至少一种管理修改有关:停用软便剂或促动力剂(RR 10.25,95% CI 5.14-20.45,p < 0.001)和粪便管理装置(应用直肠袋或插入直肠管)或艰难梭菌测试(RR 6.16,95% CI 3.4-11.17,p < 0.001)。
# 表 3 腹泻管理的调整与预后
| Management modification and consequences | Patients with diarrhea* (n = 818) | No diarrhea (n = 291) | RR (95% CI) | P value |
|---|---|---|---|---|
| Any management modification, *n* (%) | 166 (20.29) | 5 (1.7) | 10.25 (5.14–20.45) | < 0.001 |
| Stool Softener held | 118 (14.4) | 4 (1.4) | ||
| Feeds held | 52 (6.4) | 0 (0) | ||
| Feeds changed | 42 (5.1) | 0 (0) | ||
| Pro-kinetic held | 21 (2.6) | 1 (0.3) | ||
| Any management consequence, *n* (%) | 171 (20.9) | 10 (3.4) | 6.16 (3.4–11.17) | < 0.001 |
| Clostridioides difficile-associated diarrhea test | 94 (11.5) | 6 (2.1) | ||
| Other consequence | 63 (7.7) | 4 (1.4) | ||
| Rectal tube inserted | 37 (4.5) | 4 (1.4) | ||
| Rectal bag applied | 17 (2.1) | 2 (0.7) |
- In this table, we present the management modifications and consequences of diarrhea (WHO definition) on individual management consequences
- RR Risk Ratio
- *Adjusted for age, sex, APACHE II score, center
| 管理的调整与预后 | 腹泻患者 * (n = 818) | 无腹泻 (n = 291) | RR (95% CI) | P 值 |
|---|---|---|---|---|
| 任何管理修改,n (%) | 166 (20.29) | 5 (1.7) | 10.25 (5.14-20.45) | < 0.001 |
| 持有粪便软化剂 | 118 (14.4) | 4 (1.4) | ||
| 保持喂食 | 52 (6.4) | 0 (0) | ||
| 更换饲料 | 42 (5.1) | 0 (0) | ||
| 保留动力学药物 | 21 (2.6) | 1 (0.3) | ||
| 任何管理后果,n (%) | 171 (20.9) | 10 (3.4) | 6.16 (3.4-11.17) | < 0.001 |
| 艰难梭状芽孢杆菌相关的腹泻测试 | 94 (11.5) | 6 (2.1) | ||
| 其他后果 | 63 (7.7) | 4 (1.4) | ||
| 插入直肠管 | 37 (4.5) | 4 (1.4) | ||
| 应用直肠袋 | 17 (2.1) | 2 (0.7) |
- 在本表中,我们介绍了腹泻(WHO 定义)对个人管理的修改和后果
- RR 风险比
- * 根据年龄、性别、APACHE II 评分、中心进行了调整
# 腹泻的临床后果
Clinical consequences of diarrhea
Patients with diarrhea (WHO definition) stayed in the ICU a median of 6.5 days (IQR 4, 12) in contrast to those without diarrhea who stayed 3.0 days (IQR 2, 4), p < 0.001. Patients with diarrhea stayed in hospital 15 days (IQR 8, 31) compared to those without who stayed 7.0 days (IQR 3, 14), p < 0.001). In the Cox regression competing risk model, diarrhea was not associated with death (HR 0.67; 95% CI 0.42–1.06; p = 0.086). However, in the parametric models using the generalized gamma distribution, diarrhea was a predictor of ICU (HR 0.76; 95% CI 0.56–0.95; p < 0.001) and hospital (HR 0.58; 95% CI 0.41–0.74; p < 0.001) discharge, i.e., people with diarrhea were less likely to be discharged earlier. Model fit statistics are shown in the appendix (Appendix Table 5).
腹泻患者(WHO 定义)在重症监护室停留的时间中位数为 6.5 天(IQR 4, 12),而没有腹泻的患者则停留 3.0 天(IQR 2, 4),p < 0.001。腹泻患者住院 15 天(IQR 8, 31),而无腹泻患者住院 7.0 天(IQR 3, 14),p < 0.001)。在 Cox 回归竞争风险模型中,腹泻与死亡无关(HR 0.67;95% CI 0.42-1.06;p = 0.086)。然而,在使用广义伽马分布的参数模型中,腹泻是 ICU(HR 0.76;95% CI 0.56-0.95;p < 0.001)和住院(HR 0.58;95% CI 0.41-0.74;p < 0.001)出院的预测因素,即腹泻患者不太可能提前出院。模型拟合统计见附录(附录表 5)。
# 讨论
Discussion
In this international multicenter prospective cohort study of 1109 critically ill patients, diarrhea was common, and the incidence varied based on the definition. Independent modifiable predictors for diarrhea included enteral nutrition, suppository use, and number of antibiotic days, while opioid use was associated with a lower occurrence of diarrhea. These predictors were consistent across definitions. Adjusted analyses found that diarrhea was associated with longer time to ICU and hospital discharge, but was statistically not associated increased hospital mortality.
在这项针对 1109 名危重病人的国际多中心前瞻性队列研究中,腹泻很常见,而且发病率根据定义的不同而不同。腹泻的独立可改变的预测因素包括肠内营养、使用栓剂和抗生素天数,而使用阿片类药物与腹泻发生率较低有关。这些预测因素在不同的定义中是一致的。调整后的分析发现,腹泻与进入 ICU 和出院的时间延长有关,但在统计上与医院死亡率的增加无关。
Variation in bowel habit definitions [4 (opens new window)] and inattention to usual bowel habits before critical illness make it challenging to identify what may be abnormal for a critically ill patient. A systematic review of constipation, diarrhea and the use of bowel protocols in the ICU identified 8 cohort studies examining diarrhea [5 (opens new window)]. Most studies were retrospective or single-center, and used the definition applied in this study of 3 or more liquid bowel movements per day. DICE-ICU is the largest prospective multicenter study conducted with the primary focus on diarrhea in this setting; it also serves as an initial study examining the differences in stool assessment metrics and definitions. A previous single-center prospective study of 1300 critically ill patients examining a wide range of conditions contributing to gastrointestinal dysfunction (i.e. vomiting, diarrhea, bowel dilation, and gastric residuals) [17 (opens new window)], documented only 14% as experiencing diarrhea [17 (opens new window)], and found that having more than 2 gastrointestinal symptoms was associated with increased mortality and a longer length of ICU stay [17 (opens new window)]. Our study focused on diarrhea specifically, rather than gastrointestinal dysfunction more generally, using 3 definitions.
肠道习惯定义的差异 [4 (opens new window)] 以及在危重病人之前不注意平时的肠道习惯,使得识别危重病人可能出现的异常具有挑战性。一项关于便秘、腹泻和在 ICU 中使用肠道协议的系统综述确定了 8 项检查腹泻的队列研究 [5 (opens new window)]。大多数研究是回顾性的或单中心的,并使用本研究中应用的定义,即每天 3 次或更多的液体排便。DICE-ICU 是最大的前瞻性多中心研究,主要关注这种情况下的腹泻;它也是研究粪便评估指标和定义差异的初步研究。之前一项针对 1300 名重症患者的单中心前瞻性研究考察了导致胃肠功能紊乱的各种情况(即呕吐、腹泻、肠道扩张和胃残余物)[17 (opens new window)],只记录了 14% 的患者有腹泻 [17 (opens new window)],并发现有 2 个以上的胃肠道症状与死亡率增加和 ICU 住院时间延长有关 [17 (opens new window)]。我们的研究着重于具体的腹泻,而不是更普遍的胃肠功能紊乱,使用了 3 个定义。
We documented fair agreement across all diarrhea definitions applied. The WHO and the Bristol Stool Chart demonstrated moderate agreement. While the WHO definition was associated with the highest incidence of diarrhea, analyses yielded several consistent predictors across diarrhea definitions. The attributable morbidity and mortality of diarrhea across definitions was similar (data not shown). While there is no clear superior definition of diarrhea for critically ill patients, the WHO definition does encompass patients with diarrhea identified by the other definitions (Appendix Fig. 2). Ensuring consistent nomenclature in practice will improve inter-professional recognition of diarrhea at the bedside, and help to advance research in this field, including the testing effective interventions to prevent and treat diarrhea.
我们记录了所有应用的腹泻定义的公平一致性。世卫组织和布里斯托尔粪便图显示了中等程度的一致性。虽然 WHO 的定义与腹泻的最高发病率有关,但分析得出的几个预测因素与腹泻的定义一致。不同定义的腹泻的发病率和死亡率相似(数据未显示)。虽然重症患者的腹泻没有明确的优势定义,但 WHO 的定义确实包括了其他定义所确定的腹泻患者(附录图 2)。确保实践中术语的一致性将提高床旁腹泻的跨专业识别度,并有助于推进该领域的研究,包括测试预防和治疗腹泻的有效干预措施。
Our findings quantify and highlight the importance of antibiotic appropriateness and minimizing the number of antibiotic days for patients in the ICU. We showed that every additional day of antibiotic exposure is associated with a 10% increased risk of diarrhea per day, after adjusting for multiple antibiotics. Antibiotic stewardship programs may help to tailor antibiotic therapy and prevent indiscriminate prescribing; whether this reduces the burden of diarrhea remains to be evaluated [25 (opens new window), 26 (opens new window)]. Our results are consistent with a prior study suggesting that diarrhea may often be iatrogenic in that antibiotics, suppositories, and enteral nutrition predispose critically ill patients to diarrhea [2 (opens new window)]; our study helps to quantify the associated the risk.
我们的研究结果量化并强调了抗生素适当性和尽量减少 ICU 患者的抗生素天数的重要性。我们表明,在调整了多种抗生素后,每多接触一天抗生素,每天腹泻的风险就会增加 10%。抗生素管理计划可能有助于调整抗生素治疗,防止乱开处方;这是否会减少腹泻的负担,还有待评估 [25 (opens new window), 26 (opens new window)]。我们的研究结果与之前的一项研究相一致,该研究认为腹泻可能经常是先天性的,因为抗生素、栓剂和肠内营养使危重病人容易发生腹泻 [2 (opens new window)];我们的研究有助于量化相关风险。
While the enteral route is the preferred method of nutrition delivery in the ICU [27 (opens new window)], it is often considered a cause of diarrhea, prompting discontinuation [13 (opens new window)], which in turn may interrupt nutritional support. Preliminary data have shown an association between high protein feeds and diarrhea compared to other types of enteral nutrition [28 (opens new window)]. In our study, enteral nutrition was associated with the development of diarrhea. Post hoc analysis of nutritional composition suggested that high osmolality feeds or high fiber feeds were associated with diarrhea, rather than general exposure to enteral nutrition. Further research is needed on the association between diarrhea, different feeding formulae and feeding schedules (e.g., continuous or intermittent bolus).
虽然肠道途径是 ICU 中首选的营养输送方式 [27 (opens new window)],但它常常被认为是腹泻的原因,促使患者停用 [13 (opens new window)],这反过来又可能中断营养支持。初步数据显示,与其他类型的肠道营养相比,高蛋白饲料与腹泻之间存在关联 [28 (opens new window)]。在我们的研究中,肠内营养与腹泻的发生有关。营养成分的事后分析表明,高渗透压饲料或高纤维饲料与腹泻有关,而不是一般的肠内营养暴露。需要进一步研究腹泻、不同的喂养配方和喂养计划(如连续或间歇性栓塞)之间的关联。
This study documented several interventions that are initiated in response to diarrhea including altering or holding enteral nutrition, changing medications, investigating an infectious etiology, and rectal appliance management. These interventions have implications for patients and the health care system. If feeds are held frequently, this may exacerbate caloric and protein deficits. Frequent CDAD testing, although congruent with recent guidelines suggesting heightened awareness of this infection [29 (opens new window)], incur laboratory and other costs related to contact isolation precautions for patients and clinicians until results are available.
本研究记录了针对腹泻启动的几种干预措施,包括改变或暂停肠内营养,改变药物,调查感染性病因,以及直肠器械管理。这些干预措施对患者和卫生保健系统都有影响。如果经常停止喂食,这可能会加剧热量和蛋白质的缺乏。频繁的 CDAD 检测,虽然与最近的指导方针一致,建议提高对这种感染的认识 [29 (opens new window)],但在结果出来之前,会产生与病人和临床医生的接触隔离预防措施有关的实验室和其他费用。
We found that patients who experienced diarrhea had a longer stay in the ICU and hospital, but not an increased risk of death. Previous studies have yielded conflicting results regarding the association of diarrhea with increased mortality. In a recent systematic review of prospective studies of diarrhea in the ICU, an association between mortality and ICU and hospital length of stay was found; however, included studies had relatively small sample sizes, were at moderate risk of bias and the overall certainty of evidence was low [18 (opens new window)]. Reasons for worse outcomes in patients with diarrhea seen in some studies may reflect changes in gut perfusion or altered gut microbiota during critical illness [30 (opens new window)]. Translational research has shown reduced microbiome diversity in respiratory and gastrointestinal samples correlates with higher disease severity and adverse outcomes [31 (opens new window),32 (opens new window),33 (opens new window),34 (opens new window)].
我们发现,出现腹泻的患者在重症监护室和医院的停留时间更长,但死亡的风险并没有增加。以前的研究对腹泻与死亡率增加的关系得出了相互矛盾的结果。在最近对 ICU 中腹泻的前瞻性研究的系统回顾中,发现死亡率和 ICU 及住院时间之间存在关联;但是,纳入的研究样本量相对较小,存在中等偏倚风险,总体证据的确定性较低 [[18](https://link-springer-com-443.webvpn.cams.cn/article/10.1007/s00134-022-06663-8#ref-CR18)]。一些研究中看到的腹泻患者预后较差的原因可能反映了危重病期间肠道灌注的变化或肠道微生物群的改变 [30 (opens new window)]。转化研究表明,呼吸道和胃肠道样本中的微生物群多样性减少与疾病严重程度和不良后果相关 [31 (opens new window), 32 (opens new window), 33 (opens new window), 34 (opens new window)]。
Limitations of our study include lack of mechanistic data to help explain the relationship between diarrhea and clinical outcomes. We cannot exclude the possibility of observer bias influencing patient management in response to diarrhea, or unmeasured confounders affecting analyses. The analyses of association do not indicate causation of course, and our goal was not to derive a diarrhea prediction model. Although our incidence of CDAD of 2.1% in this cohort is consistent with other ICU studies, CDAD testing was at the discretion of the ICU physician, which may lead to an underestimate of the incidence. We did not classify the appropriateness of antibiotics or analyze broad spectrum antibiotics in this study. Strengths of this study include the large sample size and heterogenous population allowing for detailed examination of predictors and outcomes. Our internal pilot study refined the study methods and calculation of the sample size for multivariable regression. We published our methods and analysis plan in a peer-review journal [19 (opens new window)] enhancing the transparency of this report. We believe that the modifications to the protocol enhanced the robustness of these analyses. We enrolled consecutive, critically ill patients in both academic and community ICUs with international representation, enhancing the generalizability of the findings. Based on additional stakeholder input, we have presented our results as risk ratios instead of odds ratios (per protocol) to facilitate interpretability.
我们研究的局限性包括缺乏有助于解释腹泻和临床结果之间关系的机制性数据。我们不能排除观察者偏差影响患者对腹泻的处理,或未测量的混杂因素影响分析的可能性。当然,关联分析并不表示因果关系,我们的目标也不是为了得出腹泻预测模型。尽管我们在本队列中的 CDAD 发生率为 2.1%,与其他 ICU 研究一致,但 CDAD 检测是由 ICU 医生决定的,这可能导致对发生率的低估。在这项研究中,我们没有对抗生素的适当性进行分类,也没有对广谱抗生素进行分析。本研究的优势包括大样本量和异质人群,可以对预测因素和结果进行详细检查。我们的内部试点研究完善了研究方法和多变量回归的样本量的计算。我们在同行评议的杂志上发表了我们的方法和分析计划 [19 (opens new window)],提高了本报告的透明度。我们相信,对方案的修改增强了这些分析的稳健性。我们在学术界和社区 ICU 中连续招募危重病人,具有国际代表性,增强了研究结果的普遍性。根据其他利益相关者的意见,我们将结果以风险比的形式呈现,而不是以赔率的形式呈现(根据协议),以方便解释。
Our study may serve as a foundation for further work in refining a definition for diarrhea that is easily applied at the bedside. A universal validated definition of diarrhea in this population could be useful for inter-professional practice, to inform translational and clinical research on enteric infectious diseases, malabsorption, and gastrointestinal dysfunction. Future investigations should examine whether addressing modifiable predictors may prevent diarrhea and impact favorably on patient-important outcomes. Additional studies on gastrointestinal dysbiosis in critical illness may yield information on propensity to develop diarrhea and its attributable morbidity and mortality. Economic analyses would quantify the resources associated with diarrhea, which lead to bedside interventions by nurses, dieticians and pharmacists, diagnostic tests, and increased use of consumables, such as gowns and other personal protective equipment.
我们的研究可以作为进一步完善腹泻定义的基础,使之易于在床边应用。在这一人群中,一个普遍有效的腹泻定义可能有助于跨专业的实践,为肠道传染病、吸收不良和胃肠道功能紊乱的转化和临床研究提供信息。未来的调查应研究解决可改变的预测因素是否可以预防腹泻,并对病人的重要结果产生有利影响。对危重病人的胃肠道菌群失调的额外研究可能会产生有关腹泻倾向及其可归因的发病率和死亡率的信息。经济分析将量化与腹泻相关的资源,这些资源导致护士、营养师和药剂师的床边干预、诊断测试,以及增加消耗品的使用,如长袍和其他个人防护设备。
In conclusion, diarrhea is common among critically ill patients, and the incidence varies based on the definition employed. Modifiable diarrhea predictors include enteral nutrition and duration of antibiotic exposure. Further studies are needed to evaluate whether modifying these factors reduces the incidence of diarrhea, and to determine the impact on healthcare costs.
总之,腹泻在危重病人中很常见,其发生率根据采用的定义而不同。可改变的腹泻预测因素包括肠道营养和接触抗生素的时间。需要进一步的研究来评估修改这些因素是否会降低腹泻的发生率,并确定对医疗费用的影响。
