 丙泊酚对狒狒脑循环和自身调节的影响
丙泊酚对狒狒脑循环和自身调节的影响
# 丙泊酚对狒狒脑循环和自身调节的影响
Effect of Propofol on Cerebral Circulation and Autoregulation in the Baboon
Van Hemelrijck, Jan MD; Fitch, William MD; Mattheussen, Maria MD; Van Aken, Hugo MD; Plets, Chris MD; Lauwers, Thierry MD Effect of Propofol on Cerebral Circulation and Autoregulation in the Baboon, Anesthesia & Analgesia: July 1990 - Volume 71 - Issue 1 - p 49-54
DeepL 翻译# 摘要
The purpose of this study was to investigate the effect of propofol on cerebral blood flow, cerebral metabolism, and cerebrovascular autoregulatory capability. Seven anesthetized baboons were given propofol at three different infusion rates. An infusion of 3 mg.kg-1.h-1 caused minimal changes, but infusion rates of 6 and 12 mg.kg-1.h-1 decreased cerebral blood flow by 28% and 39%, respectively. The changes in cerebral metabolic rate of oxygen were not statistically significant. However, with the two higher infusion rates, there was a trend toward decrease, by 5% and 22%, respectively, for the cerebral metabolic rate of oxygen, and by 18% and 36% for the cerebral metabolic rate of glucose. A 25-30 mm Hg increase in arterial blood pressure had no influence on cerebral blood flow. Replacement of nitrous oxide by nitrogen had no significant influence on cerebral blood flow or metabolism.
本研究的目的是调查丙泊酚对脑血流、脑代谢和脑血管自动调节能力的影响。给 7 只麻醉的狒狒以三种不同的输液速度注射丙泊酚。3mg.kg-1.h-1 的输注引起的变化很小,但 6 和 12mg.kg-1.h-1 的输注率分别使脑血流量减少 28% 和 39%。大脑氧气代谢率的变化没有统计学意义。然而,在两个较高的输液速度下,脑氧代谢率有下降的趋势,分别为 5% 和 22%,而脑葡萄糖代谢率则下降了 18% 和 36%。动脉血压增加 25-30 毫米汞柱对脑血流没有影响。用氮气替代氧化亚氮对脑血流和代谢没有明显影响。
It is concluded that propofol causes a dose-dependent decrease in cerebral blood flow. However, the study does not prove that this decrease in cerebral blood flow is accompanied by the same degree of decrease in cerebral metabolism. Further studies are clearly needed to clarify propofol's influence on the coupling between cerebral metabolism and blood flow. The physiologic responsiveness of the cerebral circulation to alterations in arterial pressure is well preserved. Propofol appears to prevent the metabolic stimulation and increased cerebral blood flow that has been associated with the administration of nitrous oxide.
结论是,丙泊酚会引起剂量依赖性的脑血流减少。然而,该研究并没有证明这种脑血流的减少伴随着同样程度的脑代谢的减少。显然需要进一步的研究来澄清丙泊酚对脑代谢和血流之间的耦合的影响。大脑循环对动脉压改变的生理反应性得到了很好的保留。丙泊酚似乎可以防止代谢刺激和脑血流的增加,而这与施用氧化亚氮有关。
Key Words: ANESTHETICS, INTRAVENOUS-propofol. BRAIN, BLOOD FLOW-propofol.
关键字:麻醉剂,静脉注射用 - 丙泊酚。大脑,血流 - 丙泊酚。
# 序言
The use of nitrous oxide (N2O) and volatile anesthetics in neuroanesthesia has been questioned because of their effects on cerebral circulation and metabolism. The availability of a total intravenous anesthetic technique that could provide a predictable depth of anesthesia and a rapid postoperative recovery would be a useful alternative to conventional inhalation techniques. Ideally, the coupling of cerebral blood flow and metabolism and the autoregulation of the cerebral circulation should not be affected by the anesthetic.
由于氧化亚氮(N2O)和挥发性麻醉剂对脑循环和代谢的影响,在神经麻醉中的使用受到了质疑。如果有一种全静脉麻醉技术,能够提供可预测的麻醉深度和快速的术后恢复,将是传统吸入技术的有效替代。理想情况下,脑血流和代谢的耦合以及脑循环的自动调节不应受到麻醉剂的影响。
The pharmacokinetic properties of propofol make the drug suitable for maintenance of anesthesia by intravenous infusion (1). Propofol decreases both cerebral metabolism and cerebral blood flow (2,3), whereas CO2 reactivity is preserved (3). However, the effect of propofol on cerebrovascular autoregulation has not been systematically studied.
丙泊酚的药代动力学特性使该药适合于通过静脉输注维持麻醉(1)。丙泊酚会降低脑代谢和脑血流(2,3),而 CO2 反应性则得以保留(3)。然而,丙泊酚对脑血管自动调节的影响还没有得到系统的研究。
The present study was undertaken to evaluate the effect of different infusion rates of propofol on cerebral metabolism and circulation and on circulatory autoregulation in the baboon. In addition, the effect of N2O on cerebral blood flow, metabolism, and intracranial pressure during propofol infusions was investigated.
本研究是为了评估不同输注率的异丙酚对狒狒的脑代谢和循环以及循环系统自动调节的影响。此外,还研究了 N2O 对丙泊酚输注期间脑血流、代谢和颅内压的影响。
# 方法
This study protocol was approved by the authors institutional animal investigation committee, and the experiments were performed according to our institution s standards for laboratory animal care. Seven young adult baboons (12-17 kg) were anesthetized with 7.5 mg/kg IV thiopental after tranquilization with 1 mg/kg IM phencyclidine. Anesthesia was subsequently maintained with 70% N2O in oxygen (O2) supplemented with 2 mg IM phencyclidine and 100 mg IM succinylcholine every 30 min (4). The trachea was intubated and ventilation was controlled (Sulla Ventilator, Drager) to maintain CO2 tension between 38 and 42 mm Hg as assessed by the continuous measurement of end-tidal CO2 concentration (Nelcor N 1000) and intermittent blood gas analysis (ABL 11). Correction was made, where necessary, for any temperature difference between the animal and the electrode system of the blood gas analyzer.
本研究方案经作者所在机构动物调查委员会批准,实验按照本机构的实验动物护理标准进行。7 只年轻的成年狒狒(12-17 公斤)在用 1 毫克 / 公斤 IM 苯环利定镇静后,用 7.5 毫克 / 公斤静脉硫喷妥麻醉。随后用 70% 的氧气中的 N2O(O2) 维持麻醉,每 30 分钟补充 2 毫克 IM 苯环利定和 100 毫克 IM 琥珀胆碱 (4)。气管插管,控制通气(Sulla Ventilator,Drager),使 CO2 张力保持在 38 和 42 毫米汞柱之间,通过连续测量潮末 CO2 浓度(Nelcor N 1000)和间歇性血气分析(ABL 11)评估。必要时,对动物和血气分析仪的电极系统之间的任何温度差异进行校正。
A catheter was inserted into the femoral artery for direct measurement of the arterial pressure. A balloon- tipped flow-directed pulmonary artery thermodilution catheter (5F gauge, Edwards Laboratories) was introduced through the femoral vein to the pulmonary artery for measurement of pulmonary artery pressure, pulmonary capillary wedge pressure, and cardiac output using a thermodilution technique (Cardiac Output Computer, Edwards Laboratories). Additional catheters were introduced into the contralateral femoral vein for administration of fluids (3 mL.kg-1.h-1 , saline and Ringer s lactate) and into an arm vein for administration of propofol. A catheter was introduced in the lateral ventricle through a burr hole for continuous measurement of intracranial pressure.
将一根导管插入股动脉以直接测量动脉压力。通过股静脉向肺动脉引入一根带球囊的流向肺动脉热稀释导管(5F 规格,Edwards 实验室),用于测量肺动脉压力、肺毛细血管楔压,以及使用热稀释技术测量心输出量(心输出量计算机,Edwards 实验室)。另外在对侧股静脉引入导管以输液(3 mL.kg-1.h-1,生理盐水和林格乳酸盐),并在手臂静脉引入导管以注射丙泊酚。在侧脑室中通过一个钻孔引入一根导管,用于连续测量颅内压。
Systemic arterial, right atrial, pulmonary arterial, sagittal sinus venous, and intracranial pressures were continuously monitored (Could Statham Transducer, Heilige). All pressures were zero-referenced to the external auditory meatus. Mean arterial pressure (MAP), mean right atrial pressure, mean pulmonary artery pressure, intracranial pressure (ICP), and sagittal sinus venous pressure were calculated by electronic integration of the transducer signal. The electrocardiogram was continuously monitored. Body temperature was measured from the thermistor of the thermodilution catheter and maintained within normal limits (36°-38°C) using heating lamps.
全身动脉、右心房、肺动脉、矢状窦静脉和颅内压力被连续监测(Could Statham Transducer, Heilige)。所有的压力都以外耳道为零参考。平均动脉压(MAP)、平均右心房压、平均肺动脉压、颅内压(ICP)和矢状窦静脉压是通过传感器信号的电子积分来计算的。心电图被连续监测。体温由热稀释导管的热敏电阻测量,并使用加热灯将体温维持在正常范围内(36°-38°C)。
To measure cerebral blood flow (CBF), xenon 133 was injected in the right internal carotid artery through the linguofacial trunk after all other branches of the external carotid artery had been ligated distally. After removal of the parietal muscles, CBF was determined from the height/area equation by monitoring the peak count and the rate of clearance by external scintillation counting over the right parietal area (5).
为了测量脑血流(CBF),在远端结扎颈外动脉的所有其他分支后,通过舌面干向右颈内动脉注射氙气 133。移除顶叶肌肉后,通过监测右顶叶区域的峰值计数和外部闪烁计数的清除率,从高度 / 面积方程中确定 CBF(5)。
Arterial and cerebral venous oxygen contents (ABL 11) and glucose concentrations were measured simultaneously, and cerebral metabolic rates for oxygen (CMRo2) and glucose (CMRgluc) were calculated as follows: CMRo2 = CBF x (Cao2 - Cvo2) and CMRgluc = CBF X arteriovenous glucose concentration difference .
同时测量动脉和脑静脉氧含量(ABL 11)和葡萄糖浓度,并按以下方法计算氧气(CMRo2)和葡萄糖(CMRgluc)的脑代谢率。CMRo2 = CBF x (Cao2 - Cvo2),CMRgluc = CBF X 动静脉葡萄糖浓度差。
After the determination of baseline values-i.e., under 70% N2O in O2 and phencyclidine-an intravenous loading dose of 1 mg/kg propofol was given and an intravenous infusion of the drug at a rate of 3 mg.kg-1.h-1 was started for 30 min before all measurements were obtained using this dose of propofol. Subsequently the infusion rate was increased to 6 mg.kg-1.h-1 for 30 min; again, all necessary measurements were obtained while using this dose and the dose of 12 mg.kg-1.h-1. The effects of the infusions of propofol were investigated in association with the administration of N2O or nitrogen in 30% O2 — the sequence of the administrations of the N2O/ air being randomized. Measurements of the variables of interest were obtained with each infusion rate of propofol and in relation to the withdrawal/addition of N2O.
在确定基线值后 -- 即在 70% 的 N2O in O2 和芬西利丁下 -- 静脉注射 1mg/kg 的异丙酚负荷剂量,并以 3mg.kg-1.h-1 的速度开始静脉输注药物,30 分钟后用此剂量的异丙酚进行所有测量。随后,输液速度增加到 6mg.kg-1.h-1,持续 30 分钟;同样,在使用该剂量和 12mg.kg-1.h-1 的剂量时获得了所有必要的测量结果。输注异丙酚的效果是在给与 N2O 或 30% O2 的氮气时进行的,N2O / 空气的给与顺序是随机的。在每次输注丙泊酚时,以及在撤出 / 加入 N2O 时,都获得了有关变量的测量。
During each measurement, CBF and cardiac output were determined, the relevant hemodynamic variables recorded, and the appropriate samples of arterial and cerebral venous blood obtained.
在每次测量中,确定 CBF 和心输出量,记录相关的血液动力学变量,并获得适当的动脉和脑静脉血样本。
The physiologic responsiveness of the cerebral circulation was assessed by noting the changes (if any) in CBF, produced by an acute increase in MAP of approximately 25 mm Hg (induced by the intravenous administration of angiotensin Ⅱ amide [Ciba]), at baseline (after control measurements were obtained) and during the continuous infusion of propofol at dose rates of 3, 6, and 12 mg.kg-1.h-1 .
通过注意 CBF 的变化(如果有的话)来评估脑循环的生理反应性,这些变化是由 MAP 急性升高约 25mmHg(由静脉注射血管紧张素 Ⅱ 酰胺 [Ciba] 引起),在基线(获得对照测量后)和连续输注异丙酚期间,剂量率为 3、6 和 12mg.kg-1.h-1。
As time constraints did not allow establishment of steady-state blood concentrations, the mean blood propofol level with each infusion rate was calculated as the mean of the levels 30 min after the start and at the middle and end of each infusion period.
由于时间的限制,无法建立稳态血药浓度,因此每个输液速度下的平均血丙酚水平被计算为开始后 30 分钟以及每个输液期中和结束时的平均水平。
Mean values and standard deviation were calculated for each variable. Statistical analysis was performed using the Friedman test and the Wilcoxon signed-rank test for differences between control measurements and measurements at the three infusion rates. The Wilcoxon signed-rank test was used to detect any statistically significant change in CBF during the autoregulation test, P < 0.05 being considered significant.
计算每个变量的平均值和标准差。使用弗里德曼检验和威尔科森签名秩检验对对照组测量值和三种输液速度下的测量值之间的差异进行统计分析。Wilcoxon 符号秩检验用于检测自动调节试验期间 CBF 的任何统计学意义上的变化,P < 0.05 被认为是显著的。
# 结果
The propofol blood level at an infusion rate of 3 mg.kg-1.h-1 was 0.6 ± 0.07 μg/mL (mean ± SD). The blood level reached 1.42 ± 46 μg/mL at an infusion rate of 6 mg.kg-1.h-1 and 2.86 ± 1.01 μg/mL at a rate of 12 mg.kg-1.h-1l.
输液速度为 3mg.kg-1.h-1 时,丙泊酚血药浓度为 0.6±0.07μg/ml(平均值 ±SD)。输液速度为 6mg.kg-1.h-1 时,血药浓度达到 1.42±46μg/mL,输液速度为 12mg.kg-1.h-1l 时,血药浓度为 2.86±1.01μg/mL。
Hemodynamic changes during the three different propofol infusion rates are summarized in Table 1. A significant decrease in MAP occurred at infusion rates of 6 and 12 mg.kg-1.h-1 with N2O (P < 0.05). Mean arterial pressure is significantly higher with air-O2 ventilation than with N2O/O2 for the 6- and 12- mg.kg-1.h-1 infusion rates. Changes in heart rate, pulmonary artery pressures, left atrium filling pressure, and cardiac output were not significant.
表 1 总结了三种不同丙泊酚输注速度时的血流动力学变化。在输液速度为 6 和 12mg.kg-1.h-1 时,N2O 的 MAP 出现明显下降(P<0.05)。在 6 和 12mg.kg-1.h-1 输注率下,空气 - O2 通气的平均动脉压明显高于 N2O/O2。心率、肺动脉压力、左心房充盈压和心输出量的变化并不显著。
Table 1. Hemodynamic Values Before and During Propofol at Three Infusion Rates With and Without N2O in Baboons (n = 7)
表 1. 狒狒在三种输液速度下,有无 N2O 时的血液动力学值(n = 7)。
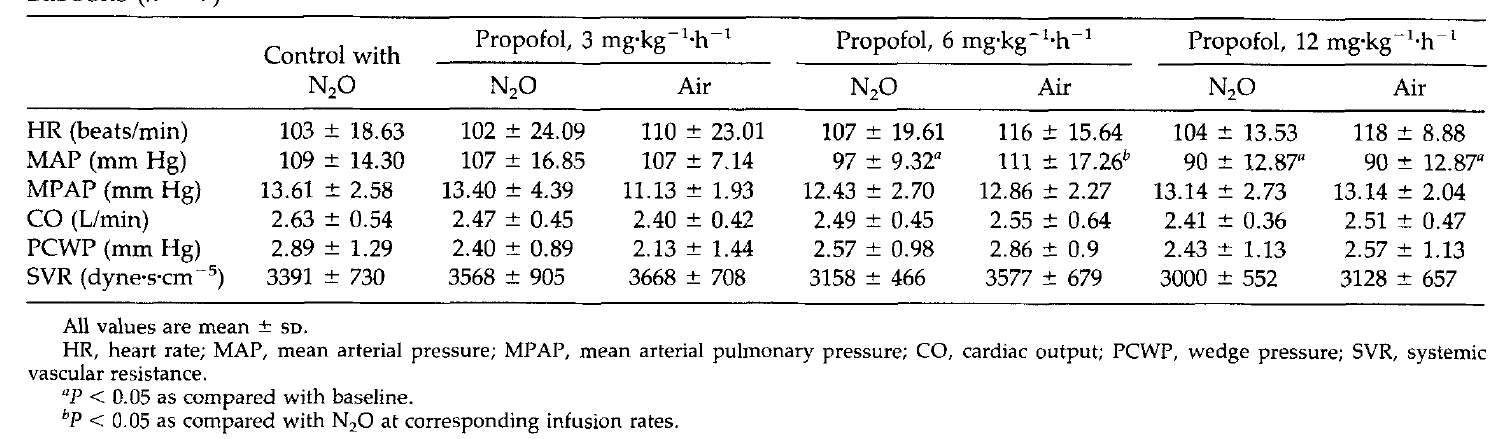
Table 2. Cerebrovascular Variables Before and During Propofol Infusion at Three Rates With and Without N2O in Baboons (n = 7)
表 2. 狒狒在三种速率下输注丙泊酚之前和期间的脑血管变量,有无 N2O(n = 7)
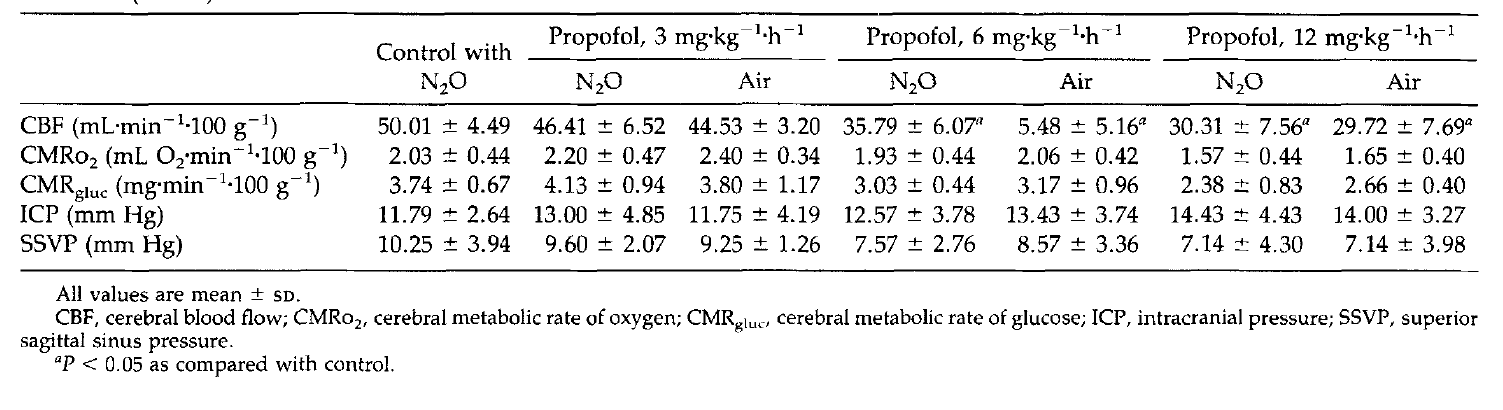
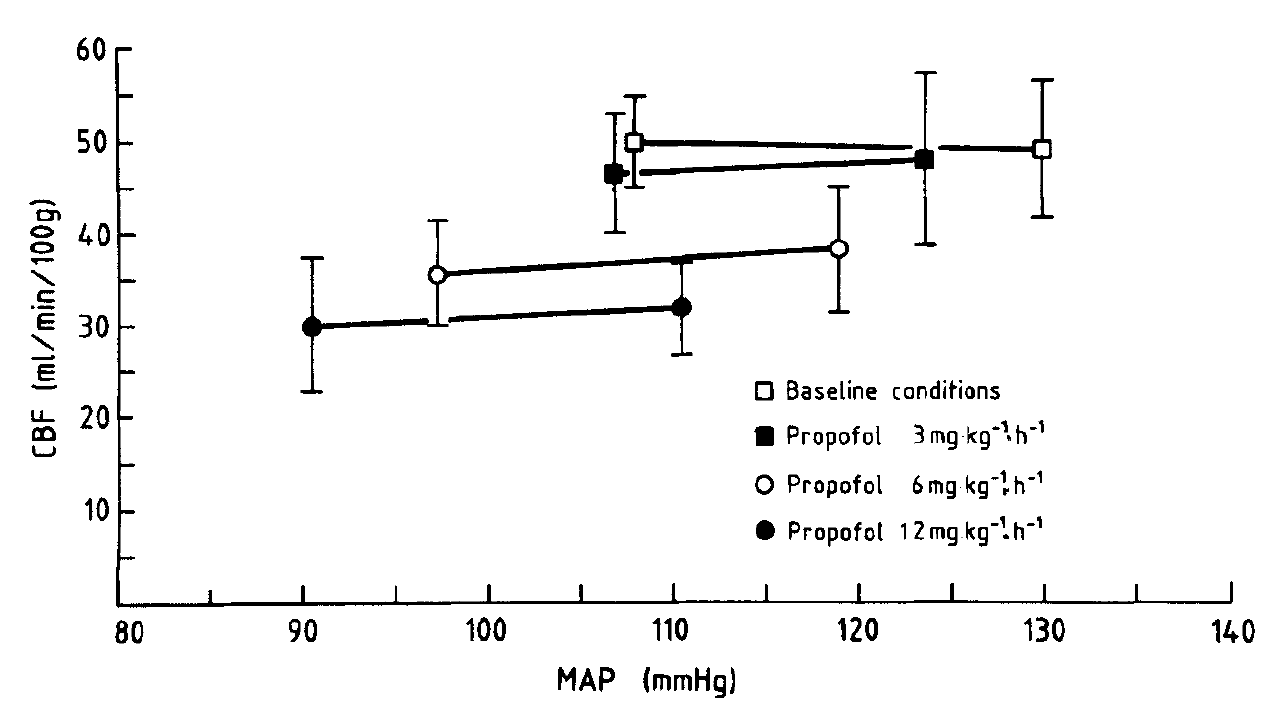
Figure 1.Cerebral blood flow (CBF) before and during acute increases in systemic arterial pressure. Cerebral blood flow was measured before and during an acute increase in MAP produced by intravenous infusion of angiotensin II amide in the absence of propofol and during infusion of propofol at rates of 3, 6, and 12 mg.kg-1.h-1
图 1. 全身动脉压急性升高前和升高期间的脑血流(CBF)。在没有异丙酚的情况下,在静脉注射血管紧张素 II 酰胺产生的 MAP 急性升高之前和期间,以及在以 3、6 和 12mg.kg-1.h-1 的速度输注异丙酚期间,测量脑血流。
Cerebrovascular variables are summarized in Table 2. Cerebral blood flow decreased significantly (P < 0.05) from 50. ± 4.5 to 46.4 ± 6.5 mL.min-1 .100 g-1 at an infusion rate of 3 mg.kg-1.h-1 with N2O. At propofol infusions of 6 and 12 mg.kg-1.h-1 with N2O CBF decreased significantly to 35.8 ± 6.1 and 30.3 ±7.6 mL/min, respectively. There was no significant difference between the CBF with air/O2 or N2O/O2 ventilation at each propofol infusion rate.
脑血管变量汇总于表 2。脑血流量明显减少(P < 0.05),从 50. 在输液速度为 3mg.kg-1.h-1 时,N2O 的脑血流量从 50.±4.5 降至 46.4 加减 6.5mL.min-1 .100g-1。在丙泊酚输注 6 和 12mg.kg-1.h-1 与 N2O 时 CBF 分别明显下降到 35.8±6.1 和 30.3±7.6mL/min。在每个异丙酚输注速度下,用空气 / O2 或 N2O/O2 通气的 CBF 没有明显差异。
There were no significant changes in ICP or sagittal sinus venous pressure with the different infusion rates. They were not influenced by the presence of N2O.
在不同的输液速度下,ICP 和矢状窦静脉压没有明显变化。它们没有受到 N2O 的影响。
Although the numerical averages of CMRo2 and CMRgluc decreased with the two higher propofol infusion rates, these decreases were not statistically significant. The metabolic rate was not altered by N2O .
虽然 CMRo2 和 CMRgluc 的数字平均值随着两个较高的异丙酚输注率而下降,但这些下降没有统计学意义。新陈代谢率没有因 N2O 而改变。
Figure 1 shows the change in CBF during an acute increase in mean arterial pressure of about 25 mm Hg before the administration of propofol and during the continuous infusion of 3, 6, and 12 mg.kg-1.h-1l propofol. Because CBF did not differ significantly from its baseline value when MAP was increased acutely either before the administration of propofol or during the three different infusion rates of propofol, it can be assumed that the cerebral vessels were responding in a normal physiologic manner to the acute alterations in systemic arterial pressure.
图 1 显示了在施用异丙酚前平均动脉压急性升高约 25mmHg 期间以及连续输注 3、6 和 12mg.kg-1.h-1l 异丙酚期间 CBF 的变化。由于在施用异丙酚之前或在三种不同的异丙酚输注速度期间,当 MAP 急性升高时,CBF 与基线值没有明显的差异,因此可以认为脑血管以正常的生理方式对全身动脉压的急性改变作出反应。
# 讨论
The time taken for propofol to reach a stable blood concentration when administered as a fixed-rate infusion exceeds 1 h (6). Steady-state blood concentrations were, therefore, not reached in this study when each measurement sequence was begun. For this reason, the propofol blood concentration for each infusion rate was calculated as the mean of three measurements.
以固定速度输注时,丙泊酚达到稳定血药浓度的时间超过 1 小时(6)。因此,在本研究中,当每个测量序列开始时,都没有达到稳定的血液浓度。因此,每个输液速度的丙泊酚血药浓度是以三次测量的平均值来计算的。
The mean propofol blood level at an infusion rate of 3 rng.kg-1.h-1 was only 0.6 ± 0.07 μg/mL. Because patients are awake after a propofol infusion when the blood concentration decreases below 1.1 μg/mL (1), effects at this drug level are probably of little if any clinical relevance. The blood propofol concentrations during the infusions at 6 and 12 mg.kg-1.h-1 were 1.42 ± 0.46 and 2.86 ± 1.01 μg/mL, respectively. A concentration of 2.97 ± 1 μg/mL has been described as being adequate for nonmajor surgery when N2O and meperidine are also used (1). Similar values have been determined for propofol infusions supplementing 67% N2O in patients premedicated with lorazepam or morphine (7,8). A concentration of 2.5 or 3 μg/mL was aimed for, with a computer-assisted infusion technique of total intravenous anesthesia (9,10).
在输液速度为 3 rng.kg-1.h-1 时,平均丙泊酚血药浓度仅为 0.6±0.07 μg/mL。因为当血药浓度下降到 1.1μg/mL 以下时,病人在输注异丙酚后是清醒的 (1),在这个药物水平上的影响可能与临床无关。在输注 6 和 12mg.kg-1.h-1 时,血液中的异丙酚浓度分别为 1.42±0.46 和 2.86±1.01μg/mL。当 N2O 和 Meperidine 也被使用时,2.97±1μg/mL 的浓度已被描述为足够用于非大手术(1)。在用劳拉西泮或吗啡作预处理的病人中,补充 67% N2O 的丙泊酚输液也有类似的数值(7,8)。以 2.5 或 3 微克 / 毫升的浓度为目标,采用计算机辅助输液技术进行全静脉麻醉(9,10)。
Cardiovascular variables remained remarkably stable throughout this study, with a maximal decrease in MAP of 17% at a propofol infusion rate of 12 mg.kg-1.h-1 . The decrease in MAP can partly be explained by an 11% decrease in systemic vascular resistance. Cardiac output, pulmonary artery pressures, pulmonary capillary wedge pressure, and heart rate (for the combination with N2O) did not change significantly. The changes in circulatory variables are in agreement with other studies on propofol infusions in healthy subjects (11-13). The absence of an increase in heart rate in response to a decrease in blood pressure during propofol infusions has been ascribed to a central sympatholytic and/or vagotonic mechanism (14). An increase in MAP and systemic vascular resistance with air/O2 as compared with N2O/O2 ventilation for the 6- and 12-mg.kg-1.h-1 infusion rates can probably be explained by an increase in sympathetic activity, due to lighter planes of anesthesia. In none of the animals was blood pressure out of the presumed cerebrovascular autoregulatory limits at any time.
在整个研究过程中,心血管变量保持明显的稳定,在丙泊酚输注速度为 12mg.kg-1.h-1 时,MAP 最大下降了 17%。MAP 的下降可以部分解释为全身血管阻力下降了 11%。心输出量、肺动脉压力、肺毛细血管楔压和心率(与 N2O 结合时)没有明显变化。循环变量的变化与其他关于健康受试者输注丙泊酚的研究一致(11-13)。在丙泊酚输注期间,心率没有因血压下降而增加,这被归因于中枢交感神经和 / 或迷走神经的机制(14)。与 N2O/O2 通气相比,在 6 和 12-mg.kg-1.h-1 输注率下,MAP 和全身血管阻力的增加,可能是由于较轻的麻醉平面导致交感神经活动增加。没有任何动物的血压在任何时候超出了假定的脑血管自动调节的范围。
A decrease in ICP has been described with 1 mg/kg IV propofol in patients with intracerebral injuries (15). A decrease in CBF and hence in cerebral blood volume can significantly diminish ICP when cerebral compliance is reduced; however, with normal cerebral compliance, changes in CBF have little influence on ICP.
在脑内受伤的病人中,用 1 毫克 / 公斤的异丙酚静脉注射,ICP 有所下降(15)。当脑顺应性降低时,CBF 的减少以及脑血容量的减少可以明显降低 ICP;但是,在脑顺应性正常的情况下,CBF 的变化对 ICP 的影响很小。
A reduction in CBF proportional to the propofol infusion rate was observed. Although this reduction was minimal durin the 3-mg.kg-1.h-1 infusion, the 6- and 12-mg.kg-1.h-1 infusion rates resulted in reductions of 28% and 39%, respectively. A reduction in CBF of 51% has been reported in coronary artery bypass patients with an infusion rate of 12 mg.kg-1.h-1 (3). Presumably, the difference in degree of CBF reduction can be explained by a different anesthetic background and by eventually differing blood concentrations (not measured in the human study), as well as species differences. A 27.6% reduction in CBF was described in humans given a propofol infusion designed to produce a stable blood concentration of 4 μg/mL with N2O and 0.5% enflurane as background anesthetics (2). The smaller decrease in CBF in spite of the higher expected blood levels can probably be partly assigned to the background anesthetic, as enflurane causes a reduction in cerebral vascular resistance (16) and could thereby modify the CBF-lowering effect of propofol.
观察到 CBF 的减少与丙泊酚的输注速度成正比。虽然这种减少在 3-mg.kg-1.h-1 输注期间是最小的,但 6 和 12-mg.kg-1.h-1 输注率分别导致了 28% 和 39% 的减少。据报道,在冠状动脉旁路患者中,输液速度为 12mg.kg-1.h-1 时,CBF 减少 51%(3)。据推测,CBF 减少程度的差异可由不同的麻醉剂背景和最终不同的血液浓度(在人类研究中没有测量),以及物种差异来解释。据描述,在人类的 CBF 减少 27.6%,旨在产生一个稳定的血液浓度为 4 微克 / 毫升,N〜2〜O 和 0.5%恩氟拉作为背景麻醉剂(2)的丙泊酚输注。尽管预期的血药浓度较高,但 CBF 的下降幅度较小,这可能部分归因于背景麻醉剂,因为恩氟拉会导致脑血管阻力的降低(16),从而改变丙泊酚的 CBF 降低效应。
The cerebral metabolic rates for oxygen and glucose did not change significantly with the 6- and 12-mg.kg-1.h-1 infusion rates, although the numerical means decreased by 5% and 22%, and 18% and 36%, respectively. Apparently, the decrease in CBF caused by propofol is incompletely coupled to a comparable decrease in cerebral metabolism. This raises concern that propofol may decrease CBF more than O2 demand. However, one animal had an unexplained abnormally low cerebral metabolic rate (CMRo2 1.41 mL O2.min-1 .100 g-1; CMRgluc 2.65 mg..min-1 .100 g-1)with a normal CBF (58.94 mL.min-1 .100 g-1 ) under baseline conditions. Its cerebral metabolism increased during the experiment. Omitting the data on cerebral metabolism of this study animal results in a significant decrease in CMRo2 of 15% and 36%, and a significant decrease of CMRgluc of 20% and 44% for the 6- and 12- mL.kg-1.h-1 infusion rates, respectively. Second, we acknowledge a potential error introduced by our calculation of CMRo2 and CMRgluc. This calculation assumes that CBF in the region under the scintillation detector changes uniformly in response to propofol as does the arteriosagittal sinus oxygen content difference. However, regional differences may exist, and the method of measuring CBF may overestimate propofol's influence on global CBF. A 36% reduction in CMRo2 was measured in patients before coronary artery surgery, during a propofol infusion of 12 mg.kg-1.h-1 (3).
氧和葡萄糖的脑代谢率在 6 和 12-mg.kg-1.h-1 的输注率下没有明显的变化,尽管数字平均值分别下降了 5% 和 22%,以及 18% 和 36%。显然,丙泊酚引起的 CBF 下降与脑代谢的相应下降是不完全耦合的。这引起了人们的关注,即丙泊酚可能比 O2 需求更多地减少 CBF。然而,有一只动物在基线条件下有一个无法解释的异常低的脑代谢率(CMRo2 1.41 mL O2.min-1 .100 g-1;CMRgluc 2.65 mg.min-1 .100 g-1),而 CBF 正常(58.94 mL.min-1 .100 g-1 )。在实验过程中,其脑部代谢增加。省略该研究动物的脑代谢数据,在 6 - 和 12-mL.kg-1.h-1 的输液速度下,CMRo2 明显下降 15% 和 36%,CMRgluc 明显下降 20% 和 44%。第二,我们承认我们对 CMRo2 和 CMRgluc 的计算引入了一个潜在错误。该计算假设闪烁探测器下区域的 CBF 在对异丙酚的反应中均匀变化,就像动脉矢状窦含氧量差异一样。然而,区域差异可能存在,测量 CBF 的方法可能高估了丙泊酚对全球 CBF 的影响。在冠状动脉手术前的患者中,在丙泊酚输注 12mg.kg-1.h-1 期间,测得 CMRo2 减少 36%(3)。
In spite of the fact that N2O increases CMRo2 and CBF (17,18), we were unable to detect any significant changes in cerebral metabolism or CBF when N2O was discontinued during the three propofol infusions. These data suggest that propofol obtunds the metabolic activation and subsequent increase in CBF which may be associated with the administration of N2O. In contrast, a 10% increase in CBF has been described in the rabbit when N2O was added to a pentobarbital-fentanyl anesthetic (19). Nevertheless, the cerebral metabolic stimulating effects of N2O can be blocked by sufficient levels of background anesthesia (17,20).
尽管 N2O 会增加 CMRo2 和 CBF(17,18),但在三次异丙酚输注过程中停止 N2O 时,我们无法检测到脑代谢或 CBF 的任何明显变化。这些数据表明,异丙酚抑制了新陈代谢的激活和随后 CBF 的增加,这可能与 N2O 的管理有关。相反,当 N2O 被添加到戊巴比妥 - 芬太尼麻醉剂中时,兔子的 CBF 增加了 10%(19)。尽管如此,N2O 的脑代谢刺激作用可被足够水平的背景麻醉所阻断(17,20)。
Cerebral blood flow did not change significantly when MAP was increased acutely either before or during the administration of propofol at three different propofol infusion rates. The cerebral vessels were reacting physiologically to the imposed pressure change; propofol thus leaves the cerebrovascular autoregulatory responses to increasing MAP unaltered. Angiotensin Ⅱ itself, used to provoke the blood pressure increases, has no effect on CBF unless administered immediately adjacent to a cerebral vessel (21,22). The same autoregulation test, under similar background anesthetic conditions, is capable of detecting disturbed autoregulation with high concentrations of isoflurane and during adenosine triphosphate- induced hypotension (23,24).
在三种不同的丙泊酚输注速度下,当 MAP 急性增加时,脑血流量没有明显变化。大脑血管对强加的压力变化有生理反应;因此丙泊酚使脑血管对 MAP 增加的自我调节反应没有改变。用于引起血压升高的血管紧张素 Ⅱ 本身对 CBF 没有影响,除非紧邻脑血管给药(21,22)。在类似的背景麻醉条件下,同样的自动调节试验能够检测到高浓度异氟烷和三磷酸腺苷诱导的低血压期间的自动调节紊乱(23,24)。
The basic anesthetic technique used in this study, namely phencyclidine, N2O, and succinylcholine, has been previously used for studies on cerebral circulatory effects of drugs, including autoregulation testing (4,23-25). Because N2O, succinylcholine, and phencyclidine were given during the entire experiment, we cannot exclude some influence of these agents on systemic and cerebrovascular hemodynamics. However, because all measurements were made under similar anesthetic background conditions, it seems likely that the observed changes can be ascribed to propofol.
本研究中使用的基本麻醉技术,即苯环利定、N2O 和琥珀胆碱,以前曾被用于研究药物的脑循环效应,包括自动调节测试(4,23-25)。由于在整个实验过程中给予了 N2O、琥珀胆碱和苯环利定,我们不能排除这些药物对系统和脑血管血流动力学的一些影响。然而,由于所有的测量都是在类似的麻醉背景条件下进行的,因此,观察到的变化似乎可以归因于丙泊酚。
Because phencyclidine alone cannot be considered as a full anesthetic, it would be unethical to perform surgery on the animals without the addition of N2O. For the same reason, baseline measurements were performed including N2O in the background anesthetic. The effect of propofol on autoregulation was also tested under the same anesthetic conditions, including N2O. When propofol completed the basic anesthetic, it was possible to study the effect of the abolition of N2O.
因为单独的苯环利定不能被认为是一种完全的麻醉剂,在没有添加 N2O 的情况下对动物进行手术是不道德的。出于同样的原因,在进行基线测量时,背景麻醉剂中包括 N2O。在同样的麻醉条件下,包括 N2O,也测试了丙泊酚对自动调节的影响。当丙泊酚完成基本麻醉后,就可以研究取消 N2O 的影响了。
In conclusion, a dose-related decrease in CBF was found during propofol infusions in baboons. However, partly due to the small number of animals studied, the study failed to demonstrate unequivocally a proportional decrease in cerebral metabolism. The autoregulatory response to blood pressure changes was not impaired by propofol. The stimulatory effects of N2O on cerebral metabolism were obtunded by propofol.
总之,在狒狒的异丙酚输注过程中,发现了 CBF 的剂量相关下降。然而,部分原因是由于研究的动物数量较少,该研究未能明确地证明脑代谢的比例下降。对血压变化的自动调节反应没有受到异丙酚的影响。N2O 对脑代谢的刺激作用被丙泊酚所抑制。
